Hands-On Experience at Dartmouth-Hitchcock Medical Center
We went to the medical center at Dartmouth multiple times for various different medical activities. Both of the hands-on activities that I did there were extremely interesting and gave me a unique experience that I would not be able to get otherwise. These activities were using the laparoscopic machine and doing an ultrasound.
Simulation Laparoscopy
A Laparoscopic Surgery is a minimally-invasive surgery where a surgeon can see and operate in the abdominal cavity without opening it up completely. A small incision is made in the belly, and the surgeon inserts a laparoscope, a thin tube with a light and a camera, through this key-hole incision. Then, carbon dioxide is inserted into the patient’s belly to inflate it to let the surgeon see the organs in the abdomen better. The surgeon may make two additional incisions to insert surgical instruments so that they can perform surgery within the abdomen. Then, the surgeon watches a monitor that shows what the camera is seeing live so that they can operate on the patient with the laparoscopic forceps and graspers. It requires immense hand-eye coordination and constant training, which is where the simulation equipment that Dartmouth-Hitchcock has comes into play. The surgeons train virtually with a machine to practice these skills. We too were able to practice using the laparoscopic machine, which was easily the highlight of the entire visit to the task lab at Dartmouth-Hitchcock. It was exceedingly difficult to look at the monitor while you moved your hands, especially because every small movement was very consequential. The machine had us stack small triangular prisms with a hole in them onto a pole using the laparoscopic forceps and graspers, which I partially succeeded in. After doing this, we were also able to see the simulation equipment that doctors used in the rest of the task lab to practice various different surgical procedures such as a tracheostomy (putting a tube through the surgically made hole in the neck to help to breathe) and a bronchoscopy (putting a bronchoscope down the throat to examine airway) among others.
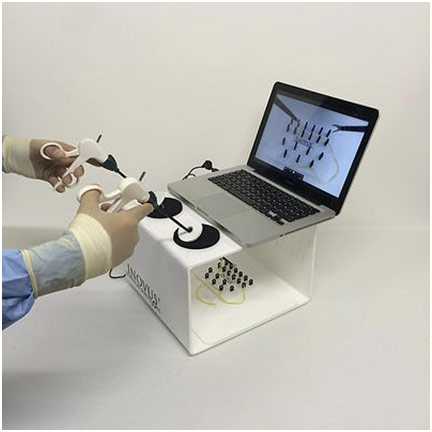
Laparoscopic Simulator
Ultrasound
This hands-on experience was taught by some nurse anesthetists (a nurse who specializes in the administration of anesthesia) on another visit to the medical center. They briefly told us about their journey of becoming a CRNA (certified registered nurse anesthetist) and how that experience was similar to the educational journey of an anesthesiologist. In many rural clinics or hospitals, CRNAs are the only medical professionals trained in delivering anesthesia available, so they do all the same work that an anesthesiologist does. Michael Hawkins, the chief nursing anesthetist at Dartmouth-Hitchcock, actually compared putting someone under anesthesia and taking care of them to a pilot taking care of the plane. The takeoff is similar to putting someone under anesthesia at the beginning of the operation. Throughout the flight, the pilot makes sure that everything is smooth and that no complications arise just as a CRNA monitors their patient during the operation. Lastly, landing the plane is like waking the patient up and making sure everything is alright following the operation. The hands-on experience that I did was looking at the brachial artery using the ultrasound. An ultrasound uses sound waves to show different tissues based on the tissue interaction with the sound waves that get reflected back to the receiver. First, I put some ultrasound gel on the ultrasound to create a fluid layer so that the ultrasound would work when I placed it on the cubital fossa. Then, I was looking at a few different vascular structures. I identified the brachial artery by placing some pressure on the ultrasound machine, which flattened the veins leaving only the artery visible. The reason the arteries do not flatten is that they have muscular walls and are part of a high-pressure system since they have to take blood away from the heart to the entire body.
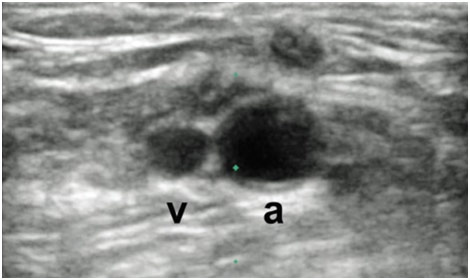
Ultrasound of Brachial Artery and Brachial Vein
Mentor Presentations
At this camp, we had five different mentors who each presented something that they have been studying or are passionate about to us. While all were extremely interesting and informative, I will talk about Jake’s and Gabriel’s presentations on anthropology and public health respectively.
Jake – Anthropology
Jake received his bachelor’s degree from SUNY New Paltz with a major in anthropology and a minor in philosophy. He told us that anthropology is the study of humans and other animals that were like humans (some of which later became humans), and everything the humans/almost humans did and still does. He gave us an example of the famous anthropologist Bronislaw Malinowski who studied the Trobriand Islanders off the coast of Papua New Guinea. These islanders would trade jewelry known as kula between all the other islands; however, none of them would ever wear it. To a common person, this may seem irrational because all the groups of islanders created and traded the kula, but none of them used it. Moreover, the trips taken to trade the kula were over large bodies of water and dangerous to say the least. By studying the islanders for a while, Malinowski began to understand that this exchange of kula was actually important for the political atmosphere as trade was seen as a demonstration of an effort to maintain a positive relationship between the different islander groups. Malinowski’s work created a paradigm shift in common people’s understandings of natives by showing that these islanders are indeed rational. He moved on to talk specifically about medical anthropology which asks questions such as “how does culture affect health?,” “what social and political factors are involved in the spread, treatment, and prevention of disease?,” and “how does health care vary across cultures.” For example, the simple behavior of washing hands was a huge breakthrough in stopping infections because it kills microorganisms that can causes diseases. However, people from different cultures rejected this idea, not because they were irrational but because they were also rational. This idea of handwashing to kill microorganisms, which they cannot see, was so crazy and drastically different to these people that they immediately rejected it without a second thought. If someone told you that by scratching your armpit and making strange noises you would cure a common cold, you would similarly reject this crazy idea and probably not even try it next time you get a cold. Therefore, there needs to be someone to build a relationship with these people, to live among them and understand their beliefs/behaviors, and to establish a rapport with them in order to make a channel of accessing that group of people’s attention. By doing so, they are able to better these people’s health and make a difference in their lives. He gave us an example of a charity called Young Heroes which provides food, clothing, and school for orphans who lost both parents to AIDS in Swaziland while also teaching them the importance of practicing safe sex to prevent the spread of HIV. However, it takes medical anthropologists to live among them and establish that relationship to teach them practices that actually oppose their king’s opinion (doesn’t believe in condoms and thinks that one must have sex with a virgin to get rid of AIDS), which is an example of a cultural barrier to health. Thus, medical anthropologists can be extremely important to make a huge shift in the health practices of different cultures.
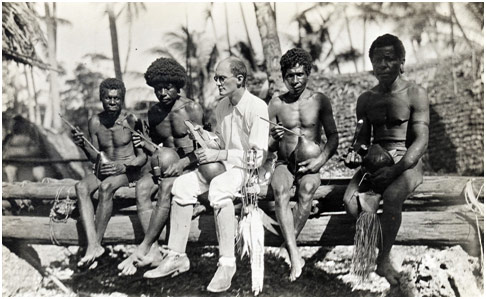
Bronislaw Malinowski with Trobriand Islanders
Gabrielle – Public Health
Gabrielle received her bachelor’s degree from Dartmouth with a major in sociology with an engineering modification. She has been accepted to graduate school at Columbia where she hopes to receive her master’s degree in public health and business. She began with an elaborate metaphor of a bridge with low walls over a fast-moving stream for the US healthcare system. The bridge represents being healthy while the river represents being sick. Only when people fall off the bridge and into the river do people fish them out of the river. Public health aims to shift healthcare delivery from downstream interventions (trying to pull people out when they are already sick) to upstream interventions instead in order to prevent people from getting sick in the first place (falling off the bridge). In order to achieve this, she explained that we must create initiatives to help all Americans falling into the stream, but we must especially help those who are more likely to fall into the stream due to the social determinants of health. These determinants include education, gender, income, race, and employment status among others, which create persistent inequalities in access and resources to health. She gave the example of a study she did of different breast cancer treatments. Breast cancer treatments include lumpectomies, which take out the tumor and some of the healthy breast tissue (least invasive); unilateral mastectomies, which remove one entire breast and the nipple; and bilateral mastectomies, which remove both breasts and the nipples (most invasive). Something interesting that came up was that black women mostly tend to have bilateral mastectomies while white women overwhelmingly tend to have lumpectomies even though there is not much evidence that points to bilateral mastectomies being more effective than lumpectomies. Bilateral mastectomies can even be worse in cases because being more invasive leads to an increased chance of infection and other complications such as death. Gabrielle told us that the doctor script to deliver the news of the breast cancer and treatment options is more tailored to white women, so it is hard for black women to understand their options and be confident in what they choose. As a public health initiative to combat this, there were groups of people who talked to black women church congregations, talking in ways they understood (with specific cultural references) to explain the different treatment options. This initiative actually reduced the rates of bilateral mastectomies among black women while not changing the mortality rates in terms of cancer but actually reducing mortality rates in terms of infection. Another interesting thing that Gabrielle told us was about one of the biggest parts of healthcare costs: non-adherence. Non-adherence is associated with poor therapeutic outcomes, the progression of the disease, and an estimated burden on billions per year in avoidable direct healthcare costs. It is estimated that 30% of the healthcare budget was wasted, and $100-300 billion of the wasted money was lost on people who do not adhere to their treatment plan. Two examples of the many reasons that patients do not comply are costs and lack of health literacy; public health initiatives can solve both of these. For example, providing food stamps that double their value when used in farmer’s markets can encourage people to eat healthier, which can help their possible hypertension for one. Moreover, having someone take the time to thoroughly explain how to use the medication correctly and the importance of doing so can help the patient’s understanding that, for example, refrigerating insulin is important to it being effective in treating diabetes.
Doctor Trying to Pull Patient out of the River
References
Bronisław Malinowski. Wikiwand, wikiwand.com/en/Bronis%C5%82aw_Malinowski. Accessed 15 Aug. 2017.
“Laparoscopy – How It’s Performed.” NHS Choices, 28 Nov. 2016, nhs.uk/Conditions/Laparoscopy/Pages/How-it-is-performed.aspx. Accessed 15 Aug. 2017.
Miller, Edward. Innova Surgical Solutions – Bringing Laparoscopic Surgery Home. Pinterest, pinterest.com/pin/404690716496941158/. Accessed 15 Aug. 2017.
Seto, Arnold. Brachial Artery and Vein. Cath Lab Digest, cathlabdigest.com/article/Ultrasound-Guidance-Upper-Extremity-Arterial-Venous-Access. Accessed 15 Aug. 2017.