Tuberculosis has been impacting human civilization for a long time. Tracing back almost 9,000 years, Tuberculosis (TB) is a bacterial infection that mainly affects the lungs and even may spread to the brain and other parts of the body if not treated. In 2021, 10.6 million people fell ill with tuberculosis. From 2020 to 2022, there was a 15.5% increase in TB cases across the United States. Due to the effects of the COVID-19 pandemic, Tuberculosis screening, prevention, and control efforts have been disrupted. While the United States has a very low incidence rate for TB, it is currently on the rise due to the high mobility of people in the past years, increasing the spread of the disease not only in America but all over the world. Tuberculosis is unique from other diseases or infections because of its high susceptibility and difficulty tracking its spread.
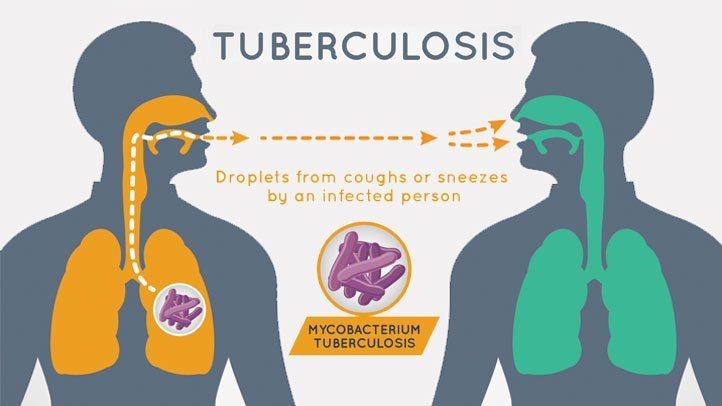
The Spread of TB
Tuberculosis is caused by a bacterium, Mycobacterium Tuberculosis. Tuberculosis transmission is more common in crowded and unsanitary conditions. It spreads rampantly in the slums of countries like India and Africa, largely due to the lack of clean water, restrooms, and widespread vaccination. Individuals with weakened immune systems, often due to other diseases such as HIV, are more susceptible to tuberculosis.
The symptoms of TB appear in a series of stages. During the primary stage, the symptoms are quite similar to those of a common flu, like low fever, tiredness, and cough. These similarities with common flu, make it especially difficult to identify Tuberculosis in patients at the primary stage. If the situation does worsen, the patient reaches the state of Latent TB infection, where the symptoms are not visible.
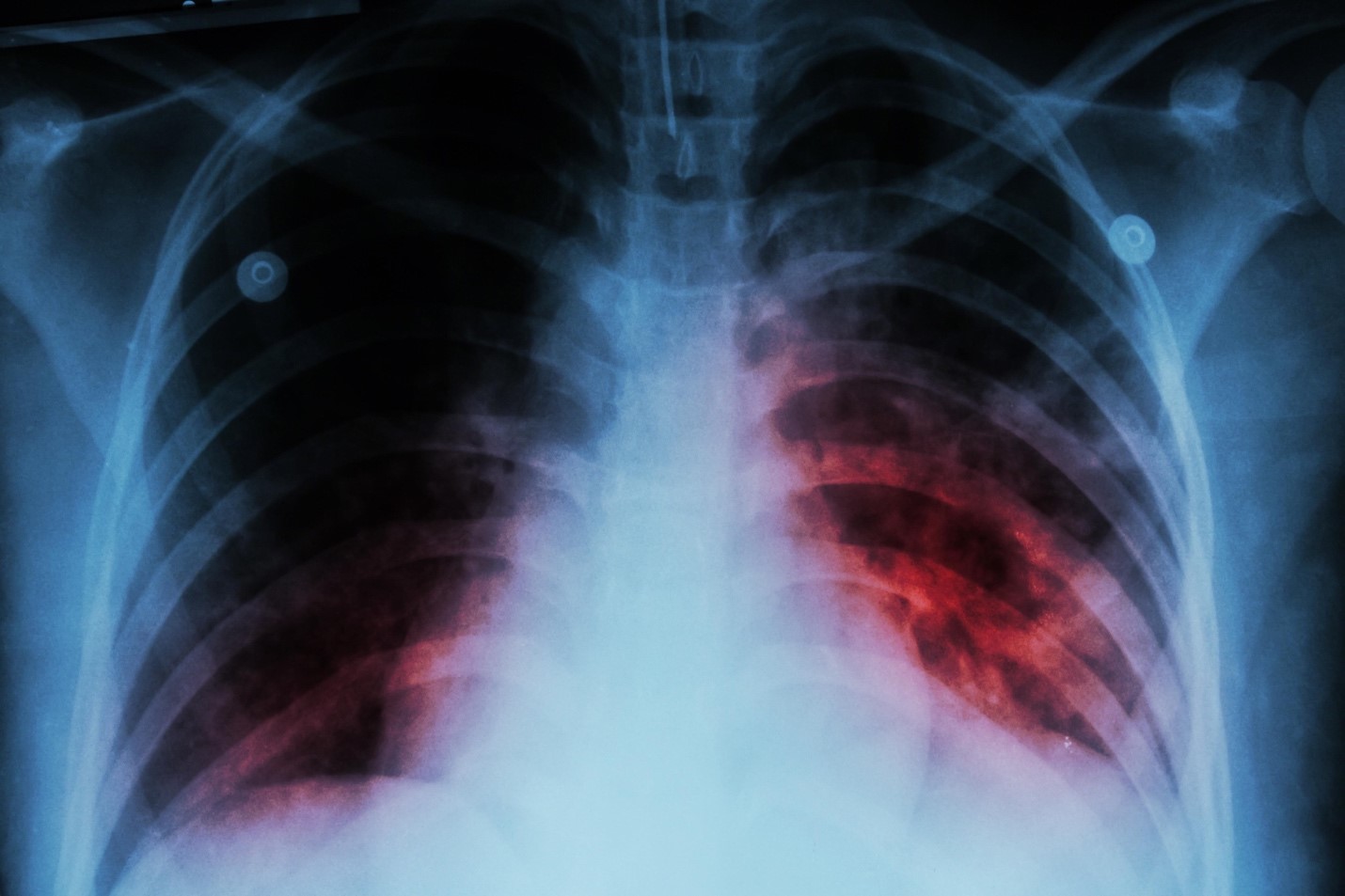
Infected TB X-Ray
During latent infection, the bacteria are in a state of dormancy. After initial infection, the immune system mounts a response against the bacteria by forming granulomas, made up of T-cells and macrophages. These granulomas keep the bacteria at bay and send them into a state of dormancy, where they are alive but not replicating. The bacteria can achieve this dormancy by forming thick waxy cell walls composed of lipids that protect the bacteria from the immune cells and drugs. The second method through which these bacteria survive is by reducing their metabolic activity, allowing them to go under the immune system’s radar.
The third stage of the infection is where we begin to see the situation go out of hand. After latent infection, a lot of the bacteria is destroyed, however, the bacterium that gets left over multiplies and attacks the lung forming cavities. When treatment is not provided, the infection spreads into other parts of the body, such as the Brain and the bones, resulting in Extrapulmonary Tuberculosis. The bacterium destroys tissue and even bones sometimes during this stage.
Most doctors check for Tuberculosis through skin testing, where a purified protein derivative is injected into the skin and depending on the skins reaction a diagnosis for TB is developed but not for active or latent. While skin testing is one the methods, there are many more such as, Chest X-Rays to identify abnormalities in the lungs such as cavities or substances that denser than air in the lungs. The most common test for TB is sputum cultures. In sputum cultures, a sample of the patient’s saliva is taken and cultured for several weeks to check the presence of Mycobacterium Tuberculosis. Another testing method that is very common in low- and middle-income countries is sputum smear microscopy. In this method, sputum is collected and examined under a microscope to detect acid-fast bacilli, a characteristic of Mycobacterium TB.
Tuberculosis can usually be treated with the help of antitubercular medications. However, when the wrong kind of medication is prescribed or the treatment is not carried out fully, it can result in Multi-Drug Resistant Tuberculosis. In some cases, when the patient begins to see the progress of taking the medicine, they refrain from continuing with the treatment due to its high cost causing them to develop MDR TB. Multi-drug resistant Tuberculosis is quite common in countries where the right kind of medication cannot be provided and when it finally is, the medication is not effective due to the body’s resistance to them.
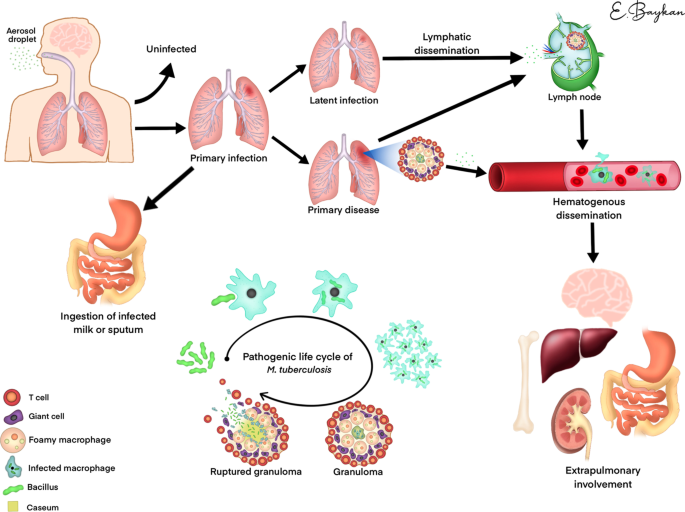
Spread of TB in the human body
While it may look like all hope is lost, many countries such as India are working towards lowering their Tuberculosis infection rates. In India, the government is currently providing free treatment to patients diagnosed with TB in its public sector as a part of its National TB Elimination Program.
Along with countries implementing health policy, medicines such as Bedaquiline play a vital role in the fight against TB. Bedaquiline is a novel antibiotic used to treat Multi-Drug Resistant Tuberculosis and Extensive Drug-Resistant Tuberculosis. Bedaquiline targets the mechanism that provides the bacteria its energy resulting in energy depletion of M. Tuberculosis. This energy depletion slows down the bacteria’s growth and replication process. Bedaquiline and its combination with other drugs provide great treatment for Tuberculosis and this combination therapy increases the treatment’s effectiveness and reduces the risk of further resistance being developed to the drugs.
Bedaquiline is an extraordinary antibiotic for targeting drug-resistant TB. However, until recently the creators, Johnson & Johnson had been enforcing their patent on the drug heavily. But now J&J has allowed 134 low and middle-income countries to produce generalized versions of Bedaquiline.
Tuberculosis has been an influence on the human experience for quite some time. Although we have developed a sense of familiarity with it, we need to do all we can to combat this disease that affects so many people yearly. TB is one of the diseases that we have yet to figure out completely but, with steps countries and companies are making with policy there is a bright future for this battle with Tuberculosis.
Bibliography
“2.1 TB Incidence.” World Health Organization, World Health Organization, www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2022/tb-disease-burden/2-1-tb-incidence. Accessed 4 Nov. 2023.
Academic.Oup.Com, academic.oup.com/cid/article/51/1/6/298996. Accessed 4 Nov. 2023.
“Drug-Resistant TB.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 13 Oct. 2022, www.cdc.gov/tb/topic/drtb/default.htm#:~:text=Multidrug%2Dresistant%20TB%20(MDR%20TB)%20is%20caused%20by%20TB,the%20treatment%20of%20MDR%20TB.
“Explore Scientific, Technical, and Medical Research on ScienceDirect.” ScienceDirect.Com | Science, Health and Medical Journals, Full Text Articles and Books., www.sciencedirect.com/. Accessed 4 Nov. 2023.
Kim, Cheon Tae, et al. “Bedaquiline and Delamanid for the Treatment of Multidrug-Resistant Tuberculosis: A Multicentre Cohort Study in Korea.” European Respiratory Society, European Respiratory Society, 1 Mar. 2018, erj.ersjournals.com/content/51/3/1702467#abstract-1.
Migliori, Giovanni Battista, et al. “Drug Resistance beyond Extensively Drug-Resistant Tuberculosis: Individual Patient Data Meta-Analysis.” European Respiratory Society, European Respiratory Society, 1 July 2013, erj.ersjournals.com/content/42/1/169.short.
professional, Cleveland Clinic medical. “Tuberculosis: Causes, Symptoms, Diagnosis & Treatment.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/11301-tuberculosis. Accessed 4 Nov. 2023.
Singh, Sarman et al. “Challenges in tuberculosis diagnosis and management: recommendations of the expert panel.” Journal of laboratory physicians vol. 7,1 (2015): 1-3. doi:10.4103/0974-2727.154778
Tb Fact Sheet Series: Sputum Collection during TB Treatment, www.dhs.wisconsin.gov/publications/p4/p47131.pdf. Accessed 4 Nov. 2023.
“Tuberculosis.” Mayo Clinic, Mayo Foundation for Medical Education and Research, www.mayoclinic.org/diseases-conditions/tuberculosis/diagnosis-treatment/drc-20351256. Accessed 4 Nov. 2023.
“Tuberculosis.” Mayo Clinic, Mayo Foundation for Medical Education and Research, www.mayoclinic.org/diseases-conditions/tuberculosis/symptoms-causes/syc-20351250. Accessed 4 Nov. 2023.
Tuberculosis Screening – Statpearls – NCBI Bookshelf, www.ncbi.nlm.nih.gov/books/NBK448205/. Accessed 4 Nov. 2023.