Humankind has made millions of discoveries and advancements across all fields in the past twenty centuries. Despite massive improvements in healthcare, many countries still need more efficient medical systems. For instance, the deficiency of insulin for diabetic patients has been a prevalent problem in American health care; in spite of the recent financial aid programs implemented by President Biden to put price caps on insulin prices, which drew my interest in analyzing how financial aid in healthcare has evolved over the decades.
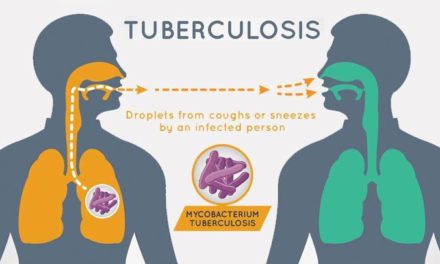
As of 2024, 30% of the countries in the world have universal healthcare systems, with the United States of America being the only developed country without universal care. Although government interference may seem like a forethought in our current times, it has not always been the government’s responsibility to provide aid for its people. As scientists discovered the causes behind various diseases, governments realized their role in protecting people from outbreaks, such as the Bubonic Plague (1346 – 1353), one of the world’s deadliest pandemics, through sanitation efforts.
Bubonic Plague (1346 – 1353)
For centuries, healthcare was considered a personal responsibility of the public. The government’s role in healthcare took a giant leap in the 19th century, when Otto Von Bismark, the prime minister of Prussia from 1873 to 1890, introduced significant changes. In the late 1800s, the people of Europe began to demand a more liberal government rather than a conservative regime. Due to internal public struggles in Prussia which later became Germany, for a more liberal government, Bismarck passed laws protecting workers’ rights and providing them with more support. Among these laws was one of the first social healthcare laws that forced employers to provide healthcare coverage to their workers. With this act, the world saw one of the first government healthcare policies to aid their people, marking the beginning of an evolution from personal healthcare to government-supported healthcare.
Otto Von Bismarck, Prime Minister of Prussia (1872 – 1890)
On July 28, 1914, World War I began and became the first global conflict which caused great devastation to both sides of the war. The majority of the loss of life during World War I was not due to the fighting on the battlefield, but rather due to the outbreak of the Spanish Flu, which lasted from 1918 to 1920. The Spanish Flu pandemic was a global influenza outbreak that claimed the lives of 21 million people exacerbated by limited understanding of the disease and inadequate resources for patient treatment. Following World War I in the twentieth century, governments saw a global economic downturn known as the Great Depression. Lasting from 1929 to 1939, the Great Depression compelled governments in the United States, the United Kingdom, Norway, Sweden, and Denmark to provide medical support to their people, as people had no money to spend on anything more than food.
As a consequence of the advancements during the Great Depression, various countries came forward with their version of the public healthcare system. In the United States, the government under Franklin D. Roosevelt passed the Social Security Act, which included healthcare benefits for the elderly, disabled children, and injured workers. While, the government of the United Kingdom focused on public health services, which included continued vaccination programs and improved sanitation to reduce the spread of infectious diseases. The Social Democratic Party in Sweden passed reforms that expanded medical care to the poor and unemployed and increased government funding for healthcare services during the economic crisis to ensure their availability to the general public. Similarly, Denmark made sure to provide healthcare to even those who were unemployed, which laid the foundation for the Danish healthcare program, which is today characterized by universal access and comprehensive coverage.
Spanish Flu (1918 – 1920)
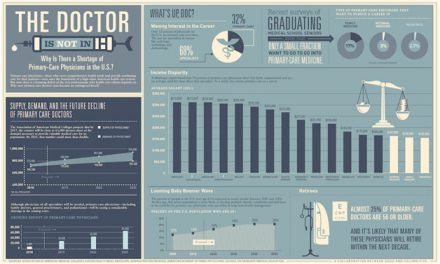
After World War II, the world was devastated. To aid in the recovery of the British people, the United Kingdom created the National Health Services, supported by taxation, to provide healthcare to everyone in the country. While the British followed the Beveridge model in Healthcare, Germany followed the Bismarck model after the chaos of the 1940s. Germany expanded and refined their model to work with healthcare funds, which are funds provided by the people for their general healthcare. In the United States, in 1965, President Lyndon B. Johnson passed the Medicare and Medicaid Act which provided healthcare insurance to the elderly especially those with a low income. Medicare and Medicaid remain the cornerstones of the American healthcare system, which continues to provide healthcare to those who cannot afford it and aid them with their chronic conditions requiring several visits to the emergency room or the hospital. Following in the footsteps of the United States, Canada passed a Medical Care Act in 1966, to provide federal funding to the provinces and territories to ensure that all people have proper access to medical care. The increased support and involvement of the government in medical care for their people allowed for great prosperity in the latter half of the twentieth century after the Second World War’s chaos. In the second half of the twentieth century, governments began taking greater control over mental health issues, by building mental institutions. Additionally, substance abuse problems were addressed using prevention, treatment, and rehabilitation services. The twentieth century also saw the development of emergency medical services, a resource that is used globally. Doctors also began receiving revised and improved education in the field of medicine and were incentivized by the government to work in rural areas to improve access to care in underdeveloped regions.
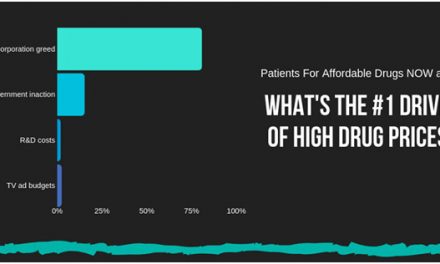
Despite the significant changes of the twentieth century, governments constantly need to work on new policies and agendas. In the modern age of medicine, with new machines and techniques to aid proper healthcare, the cost of receiving healthcare has risen significantly and mostly requires healthcare insurance in the United States. If a person does not have healthcare or Medicare or Medicaid in the United States, a simple ER visit could cost them over 700 dollars. To help with the expenses in 2010, President Obama passed the Affordable Care Act which ensured that patients receive the most cost-friendly option for insurance using insurance marketplaces, and implemented consumer protections to improve access to healthcare. Today, we see great healthcare systems all around the world, not just in the United States or Europe, but in countries like Singapore, and Hong Kong, with public and private healthcare and Japan with universal healthcare.
In 2020, the world was hit by the COVID-19 pandemic, which strained healthcare systems globally. However, the pandemic also prompted governments to improve their healthcare systems. Medical care for people with chronic diseases was made a priority during the pandemic, ensuring that patients needing immediate care received early vaccinations to continue treatment. COVID-19 bore similarities to the Spanish Flu Pandemic, a deadly global influenza pandemic from 1918 to 1920. Experiences from the Spanish Flu have provided some essential learnings to the management of healthcare during the COVID-19 pandemic and made the process manageable and more efficient. But the less fortunate were the most badly hit. The lack of jobs, lack of finances, lack of sanitary conditions, and lack of affordable healthcare made the COVID-19 pandemic unbearable for these people.
With a constantly growing population coupled with the scarcity of resources, the optimization of healthcare has become paramount. Saving resources can extend medical care to more people; paving the path towards universal healthcare. Historical events like the cholera outbreak in India during the nineteenth century, the Spanish Flu, and the COVID-19 pandemic offer valuable lessons for improving healthcare efficiency and affordability for all. The solutions to our healthcare challenges lie hidden within our past experiences, waiting to be unearthed.
Citations
Barkin K. Otto von Bismarck | Biography, Significance, Accomplishments, & Facts [Internet].
Encyclopedia Britannica. 1998. Available from: https://www.britannica.com/biography/Otto-von-Bismarck
Dowling S. Coronavirus: What can we learn from the Spanish flu? [Internet]. 2022. Available from:
https://www.bbc.com/future/article/20200302-coronavirus-what-can-we-learn-from-the-s panish-flu
Health care before the NHS [Internet]. Nuffield Trust. Available from: https://www.nuffieldtrust.org.uk/chapter/inheritance
Institute of Medicine (US) Committee for the Study of the Future of Public Health. The Future of Public Health. Washington (DC): National Academies Press (US); 1988. 3, A History of the Public Health System. Available from: https://www.ncbi.nlm.nih.gov/books/NBK218224/
Onion A. Black Death – Causes, Symptoms & Impact. HISTORY [Internet]. 2023 Mar 28; Available from: https://www.history.com/topics/middle-ages/black-death
Statutory pension insurance – German Federal Statistical Office [Internet]. [cited 2024 Jul 1].
Available from:
https://www.destatis.de/EN/Themes/Labour/Labour-Market/Quality-Employment/Dimen sion4/4_7_StatutorPensionInsurance.html#:~:text=In%20Germany%2C%20in%202022
%20all,the%20statutory%20pension%20insurance%20scheme.
The 1918 Flu Pandemic: Why It Matters 100 Years Later | Blogs | CDC [Internet]. 2018.
Available from: https://blogs.cdc.gov/publichealthmatters/2018/05/1918-flu/
Tang N, Eisenberg JM, Meyer GS. The roles of government in improving health care quality and safety. Jt Comm J Qual Saf. 2004 Jan;30(1):47-55. doi: 10.1016/s1549-3741(04)30006-7. PMID: 14738036.
Yu, S., Wan, R., Bai, L., Zhao, B., Jiang, Q., Jiang, J., & Li, Y. (2023). Transformation of chronic disease management: Before and after the COVID-19 outbreak. Frontiers in public health, 11, 1074364. https://doi.org/10.3389/fpubh.2023.1074364