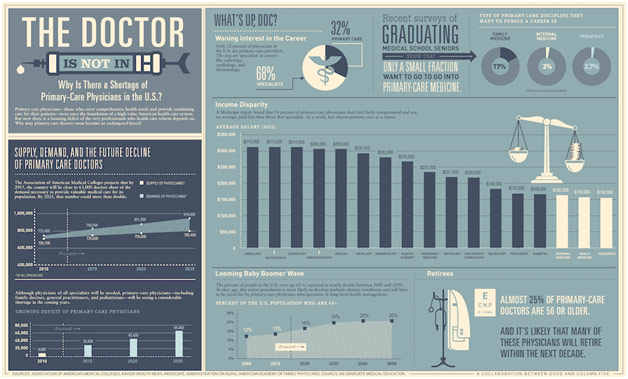
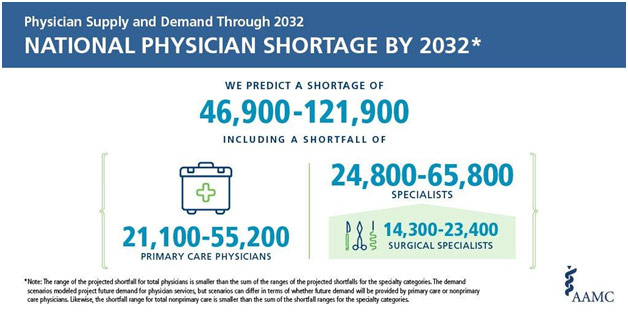
Shortages are the bane of any physician. In the wake of Hurricane Maria, the nation experienced a shortage of IV fluid as manufacturing plants in Puerto Rico were destroyed. The current COVID-19 pandemic has most prominently highlighted a shortage of personal protective equipment, from masks to gloves to gowns. For decades, however, the nation has been experiencing a more insidious shortage: a shortage of physicians themselves. By 2032, the nation could be short 122,000 physicians, and the paucity of primary care physicians (PCPs) in particular might be the most deleterious. PCPs serve as the base of the pyramid of healthcare, being the custodians of health for countless; these are the physicians who meet you at your annual checkups, the physicians who are at the vanguard of preventive medicine. In fact, people who see their PCP consistently have been found to have better health outcomes with lower costs. A shortage of PCPs thus has potentially astronomical and terrible consequences for our nation’s health. In this post, I want to delve into the causes of this devastating shortage of PCPs and discuss potential paths moving forward to ameliorate this scarcity.
Magnitude of the National Physician Shortage
Perhaps one of the most obvious reasons for the PCP shortage comes down to the economics of medical education. Medical school is undeniably expensive: in-state public medical schools cost about $37,556 a year while out-of-state private medical schools cost about $62,230 a year. It thus comes to no surprise that graduating medical students are saddled in debt: on average, $232,300 of debt, which takes these new physicians around 13 years to pay back. Debt is crippling in many ways, not only because of the interest that forces you to pay multiples of what you originally borrowed but also because of what you cannot do, from going on a vacation to buying a house, as cash beyond living expenses is often spent paying off the loan. Residency, while officially a job, pays just enough for these medical school graduates to get by, doing so because it is still training. Given the financial burden associated with becoming a physician, it comes to no surprise that medical students want to pay off their debt as soon as possible. Primary care fields, such as family medicine, pediatrics, and internal medicine, do not pay as well as more specialized fields, such as orthopedic surgery and dermatology, leading physicians struggling with debt to let money make their decision rather than personal interests. As a result, a few medical schools such as NYU and the Cleveland Clinic have made medical school entirely free to all its students so that the economics of medicine do not force a student to go into a high-paying specialty. The hope is that more of their graduates will enter primary care to help fill this devastating shortage.
Another idea that has been floated around is for the government to increase Medicare reimbursements for the important work that PCPs do so that the economic incentives of entering primary care will correspondingly increase. PCPs’ preventive medical work is often not fully appreciated because the healthcare costs had they not intervened are of course not visible. Nonetheless, the work these PCPs do holds enormous economic value and should be more fully recognized by the government. Tackling the economic incentives likely holds the greatest probability of success, but taking this path also involves enormous difficulty because these ideas are very, very expensive.
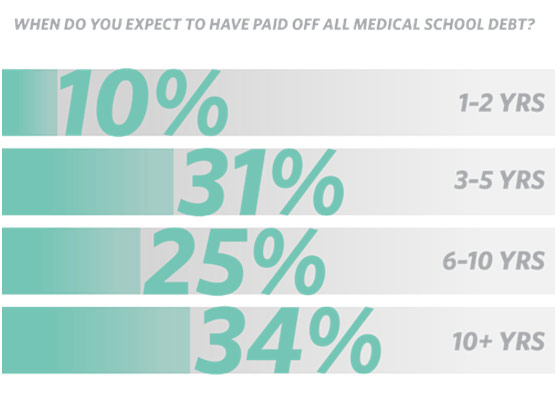
When Medical Students Expected to Have Debt Paid Off
There are a couple of other interesting medical school based approaches to tackle the PCP shortage. Allopathic medical schools, schools that provide students with an MD, have been tasked with increasing exposure to primary care to its students. For example, this might involve lengthening the mandatory rotation with internal medicine for its students, and having this rotation come early on during the formative periods of medical school. However, the PCP shortage may be better tackled by osteopathic medical schools, schools that provide students with a DO. 2019 was the first year that international medical school graduates and osteopathic doctors matched into more primary care residency physicians than allopathic doctors. Osteopathic medical schools already have an intense focus on primary care, which results in their choice of residency reflecting that training. Of course, successfully tackling this shortage will require efforts by both types of medical schools.
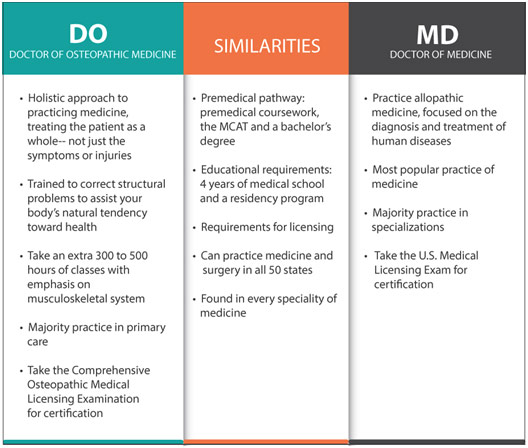
Comparison Between Osteopathic and Allopathic Physicians
The obvious solution to the shortage is to simply make more physicians. Indeed, one of the causes of this primary care physician shortage is simply that federally-funded residency positions have been capped by the government for the past 20 years. The result has been that the number of residency positions has only increased by 1% while the number of medical school positions has increased by over 50% since 2002. The potential doctors are there, but the positions to train them are not. As a result, in 2019, the Resident Physician Shortage Reduction Act was introduced to Congress to have the government create 3000 new residency positions so that thousands of new physicians could be created every year. The obvious issue with this bill is that 3000/year pales in comparison to the 122,000 physician shortage by 2032; this bill is just not enough. Perhaps worse, this bill, despite being bipartisan, might go nowhere in Congress because of the cost associated with creating 3000 new residency positions. Former New York House representative Joe Crowley tried five times to increase the number of physicians, but each time he failed. The COVID-19 pandemic may highlight the primary care physician shortage and push Congress to pass this bill, but history is not kind to the hopes of this bill.
We must, of course, perhaps prepare for a world where the decline in PCPs continues unabated, leaving the nation without enough non-specialized physicians to care for the population. One solution independent of physicians is for nurse practitioners (NPs) and physician assistants (PAs) to fill those roles. With shorter and less financially draining training, these healthcare practitioners have the training and the drive to be effective deliverers of primary care. In fact, the numbers of NPs have actually increased dramatically over the past decade, from about 120,000 in 2007 to 248,000 in 2018. One study found that NPs and PAs could fill about 70% of the roles created by the PCP shortage. This is not to suggest that NPs and PAs entirely absorb the role of primary care, but that they will provide an important supplement as physicians shift towards specialized training. Of course, challenges with this plan still persist in the form of NPs and PAs not having the legal right to practice independently in many states.
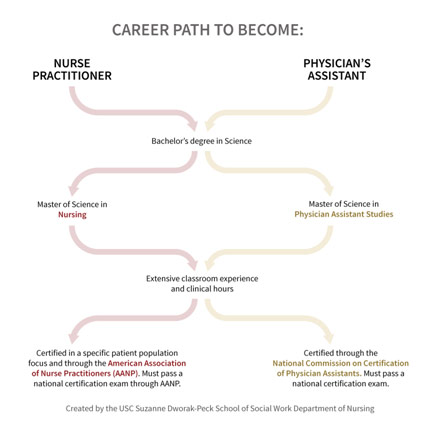
Career Path to Become a Nurse Practitioner or Physician’s Assistant
With all these potential solutions, we are playing the long game because our actions today will take decades to show their results. After all, it takes that much time for medical students to become independent practicing physicians. However, this reality just underscores the importance of decisive action as soon as possible to avoid potentially catastrophic health consequences down the road. We must make investments today in the physicians of our future.
REFERENCES
American Association for Medical Colleges. How Big Is the Projected Shortage? Twitter, twitter.com/AAMCtoday/status/1125434756328579072.
Carter, Matt. “Average Student Loan Debt.” Credible, 27 Mar. 2020, www.credible.com/blog/statistics/average-medical-school-debt/. Accessed 20 May 2020.
Heath, Sara. “NPs, PAs Could Reduce Primary Care Physician Shortage Nearly 70%.” Patient Engagement HIT, patientengagementhit.com/news/nps-pas-could-reduce-primary-care-physician-shortage-nearly-70. Accessed 20 May 2020.
Knight, Victoria. “America to Face a Shortage of Primary Care Physicians within a Decade or so.” The Washington Post, 15 July 2019, www.washingtonpost.com/health/america-to-face-a-shortage-of-primary-care-physicians-within-a-decade-or-so/2019/07/12/0cf144d0-a27d-11e9-bd56-eac6bb02d01d_story.html. Accessed 20 May 2020.
Landi, Heather. “Lawmakers Introduce Bill to Fund More Medical Residency Slots to Combat Physician Shortage, Opioid Crisis.” Fierce Healthcare, 21 Nov. 2019, www.fiercehealthcare.com/practices/federal-lawmakers-introduce-bill-to-fund-more-medical-residency-positions-to-combat. Accessed 20 May 2020.
Matthews, Melanie. Why Is There a Shortage of PCPs in the U.S.? Feb. 2013. Healthcare Intelligence Network, hin.com/blog/tag/primary-care-physician-shortage/. Accessed 20 May 2020.
MD Vs. DO: What’s the Difference in a Physician’s Title. Our Lady of the Lake, ololrmc.com/blogs/md-vs-do-whats-the-difference-in-your-physicians-title. Accessed 20 May 2020.
“Nurse Practitioner Role Grows to More than 270,000.” American Association of Nurse Practitioners, 28 Jan. 2019, www.aanp.org/news-feed/nurse-practitioner-role-continues-to-grow-to-meet-primary-care-provider-shortages-and-patient-demands. Accessed 20 May 2020.
Nurse Practitioner Vs. Physician Assistant. USC Department of Nursing, nursing.usc.edu/blog/np-vs-pa/. Accessed 20 May 2020.
“Tuition and Student Fees Reports.” American Association of Medical Colleges, www.aamc.org/data-reports/reporting-tools/report/tuition-and-student-fees-reports. Accessed 20 May 2020.
When Do You Expect to Have Paid off All Medical School Debt? Weatherby, weatherbyhealthcare.com/blog/medical-school-debt-report-2019. Accessed 20 May 2020.
Wofford, Benjamin. “We’re Devastatingly Short on Doctors. Why Doesn’t the US Just Make More?” Washingtonian, 13 Apr. 2020, www.washingtonian.com/2020/04/13/were-short-on-healthcare-workers-why-doesnt-the-u-s-just-make-more-doctors/. Accessed 20 May 2020.