From July 25th to August 2nd, I was at UC Berkeley for the NSLC Medicine and Healthcare Camp. It was an exhilarating and educational experience where I learned so much in so little time with the help of great lecturers and team advisors who helped facilitate this program. This post is the first part of a two-part series covering the highlights of this camp based on my opinion.
SFGH
We had the pleasure of going to San Francisco General Hospital for a series of 7 simulations led by various medical professionals. Each was uniquely informative and simulated a real-life scenario, making it all the more valuable; however, I will focus on a few of my favorite ones for this segment.
Vital Signs
The vital signs include pulse, respiration rate, blood pressure, and body temperature. For pulse, we checked our partner’s pulse along the carotid artery (in the neck) and learned about taking it along the radial artery (in the forearm), brachial artery (front side of the elbow), femoral artery (in the thigh), and popliteal artery (in the knee region). We counted the pulse rate for 15 seconds and then multiplied by four to get beats per minute; a normal heart rate is between 60-90 beats per minute. For respiration rate, we placed our stethoscope on our partner’s lungs to count the rate of breaths per minute, which is supposed to be between 12-20; however, you could also just count the number of times the chest rises and falls. For blood pressure, we used an automatic sphygmomanometer (blood pressure monitor) and a manual one along with a stethoscope in order to measure our partner’s blood pressure. Moreover, we learned that the average healthy blood pressure is usually 120/80 (systolic over diastolic pressure). Lastly, we measured temperature, which can be taken axillary, rectally, and aurally; however, we simply did it orally. The most accurate is the rectal temperature (through the core) while the least accurate is the axillary temperature (through the armpit); the normal temperature is 37˚C or 98.6˚F.

Taking Blood Pressure with a Manual Sphygmomanometer
Starting an IV
Next, we started an IV on a life sized dummy arm. IVs are generally set up to give fluids, nutrients, or medication to a patient intravenously because it is the quickest way possible. First, you place a tourniquet in the region between where you will be placing the IV and the heart, tying it tight to compress the arm. Next, you use antiseptic to clean the patient’s forearm and insert the IV catheter into the vein at a 30-degree angle. Once you see a flash of blood in the catheter, you withdraw the needle while keeping the angiocath in the vein. Then, you put some saline flush into the vein through the angiocath and then connect the angiocath to the IV connector extension, which goes up the IV bag. Lastly, you put the tegaderm tape to keep the IV in place.
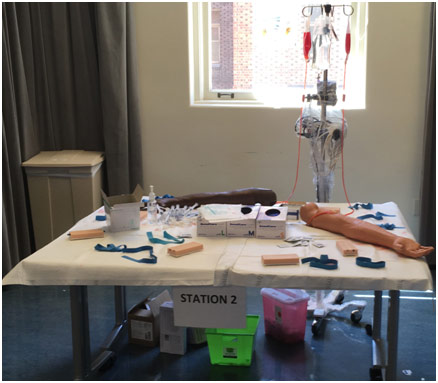
Setting up IV Station at SFGH
Intubation
Intubation is the process of opening an airway for the patient to help them breathe. We did this process for various different dummies. First, you use the manual bag and mask resuscitator to help the patient breathe. Then, you place the laryngoscope in the patient’s mouth and push the tongue to the left to be able to see the vocal cords. You then place the endotracheal (ET) tube through the patient’s mouth until the cuff is past the vocal cords. You then inflate the cuff so that there is friction and the ET tube will not come loose. Lastly, you can attach the ET tube to a manual resuscitator or a ventilator. It is important to auscultate the lungs to make sure the intubation was done correctly by looking for equal breath sounds on both sides of the lungs.
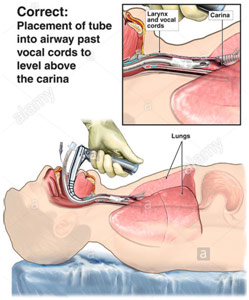
Correct Intubation Method
Head Trauma
There was a life-sized dummy that was lying in a hospital bed with severe head trauma. The first thing that we noticed was that he had differing pupil dilation, meaning that he had increasing brain pressure. This is often deadly because the skull is a closed system with only blood, brain tissue, and spinal fluid, so there is nowhere for the pressure to go. One way to relieve the pressure is a craniotomy (a surgical procedure to get to the brain); however, there is more on that later. We asked the dummy basic questions like “what year is it?” “What is your name?” and “where are you?” to check if he had any brain damage, which he did since he did not answer these questions correctly. In addition, we had to log roll him when he started to vomit so that he would not choke on his vomit. Furthermore, we had to provide him with CPR in form of 30 compressions followed by 2 breaths when he lost his pulse. Eventually, we were able to stabilize the dummy and move on to the next station.

Improper Pupil Dilation
Stop the Bleeding
One of the most dangerous bleedings is arterial bleeding because it is extremely easy to die from it because arteries are near the surface of the extremities. The most important thing to do first compresses the region that is bleeding, ideally with fibrinogen gauze that helps blood clot easier to stop the bleeding. In addition, the gauze, or whatever is used to cover the bleeding, should be tied to increase the pressure on the bleeding. If the bleeding does not stop, then a tourniquet (if physically possible) should be put to stop the blood flow to that region to stop the bleeding.
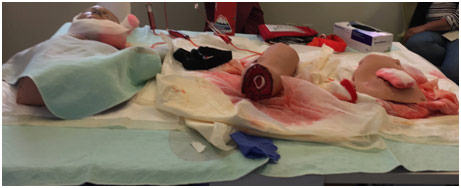
Stop the Bleeding Station at SFGH
Gladstone
Afterward, we were able to go to one of the most well respected and well-known research facilities in America: the Gladstone Institute. There we had two lectures, one about the Zika virus and another about aging, by researchers doing their post-doctorate at Gladstone.
Dr. Fontaine – Zika Virus
Zika virus is spread by the Aedes aegypti mosquito, and it mostly came into the public eye following an epidemic in Brazil right before the 2016 Rio Olympic Games. While the virus, most of the time, does not give any symptoms to a mother, it does impair the growth of developing fetuses. Babies whose mothers had Zika ended up being diagnosed with microcephaly, which is when they have a small head. This condition leads to delays in speech/movement, intellectual disability, and having seizures. Zika virus works by killing the neural stem cells, which eventually become the differentiated neuron and differentiated glial cells in the baby, so this baby does not have these neuron and glial cells. In a healthy person, there is a protein called UPF1 that destroys any improperly copied RNA, as well as anything that is not the properly copied RNA (e.g., viruses). However, the Zika virus degrades the UPF1 proteins because one ZIKV capsid binds to UPF1, so the RNA surveillance pathway is disrupted. This allows the Zika virus to kill the neural stem cells without being killed by the UPF1 protein.
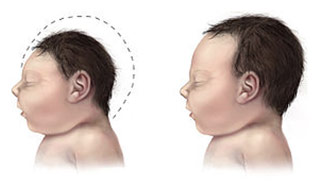
Microcephalus in Infant
Dr. Bennett – Aging
Biological age is the buildup of damage on a molecular, cellular, and tissue level for 7 distinct reasons: cell loss, division-obsessed cells, death-resistant cells, mitochondrial mutations, intracellular junk, extracellular junk, and extracellular matrix stiffening. Most diseases impact one or more of these reasons. For example, cancer is when tumorous cells divide and undergo metastasis (division-obsessed cells). Heart disease is when there is heart muscle death following a heart attack due to lack of oxygen (cell loss), clogging of arteries (intracellular and extracellular junk), and hardening of arteries (matrix stiffening). Genetic factors along with other damage (e.g., cellular metabolism, UV light, and chemical exposure) can also accelerate aging. Eventually, cells reach senescence and stop dividing, often because of telomere shortening. The cells send out a signal, inflaming the region, to get the immune system to get rid of them. However, as Dominick Burton and Valery Krizhanovsky put it, “senescent cells accumulate in tissues, either because an aging immune system fails to remove them, the rate of senescent cell formation is elevated, or both.” The current approach to combat aging is to assess each individual course of the 7 reasons one by one. In the future, it may be possible to replace, reinforce, and remove parts of the body with regular checkups to elongate life by stopping the damage before it even happens.

References
A Baby with Microcephaly (left) Compared to a Baby with a Typical Head Size. Wikipedia, en.wikipedia.org/wiki/Microcephaly. Accessed 29 Dec. 2020.
Blood Pressure Cuff – Manual. Willowbrook Medical Supplies, willowbrookmedicalsupplies.com/index.php/product/blood-pressure-cuff-manual/. Accessed 29 Dec. 2020.
Burton, Dominick, and Valery Krizhanovsky. “Physiological and Pathological Consequences of Cellular Senescence.” Cellular and Molecular Life Sciences, vol. 71, no. 22, 31 July 2014, pp. 4373-86, www.ncbi.nlm.nih.gov/pmc/articles/PMC4207941/. Accessed 29 Dec. 2020.
Correct (Endotracheal) vs. Incorrect (Esophageal) Intubation. Alamy, www.alamy.com/correct-endotracheal-vs-incorrect-esophageal-intubation-image7710490.html. Accessed 29 Dec. 2020.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4207941/
https://en.wikipedia.org/wiki/Microcephaly
http://www.alamy.com/stock-photo-correct-endotracheal-vs-incorrect-esophageal-intubation-7710490.html
http://aiyus.org/category/resource-from-internet/















