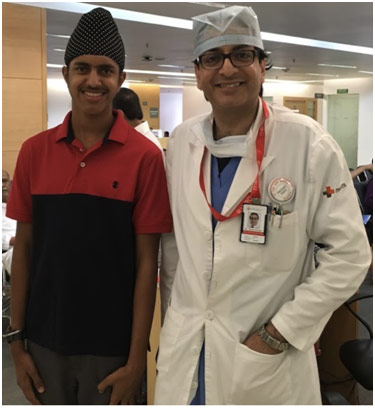
Dr. Tarun Grover is a vascular surgeon, practicing at Medanta Hospital in Gurgaon, India. He attended medical school at Gajra Raja Medical College in Gwalior, India. After completing medical school, Dr. Grover did his residency at Sir Ganga Ram Hospital. His interest in vascular surgery developed during his general surgery training as he found vascular and endovascular procedures fascinating because of newer advances at the time like minimally invasive techniques of angioplasty, EVAR (endovascular aneurysm repair), and TEVAR (thoracic endovascular aortic repair). I was able to do an internship with him over a course of ten days where I scrubbed up and observed some surgeries in the Operation Theatres (OT) as well as seeing patients in the Outpatient Department (OPD). It was a remarkable experience to see the inner workings of a hospital from a surgeon’s perspective, and it was incredibly educational since I was physically able to see many of the surgeries.
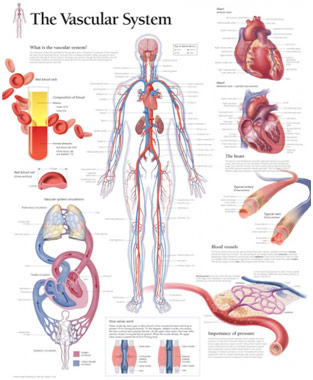
Vascular System
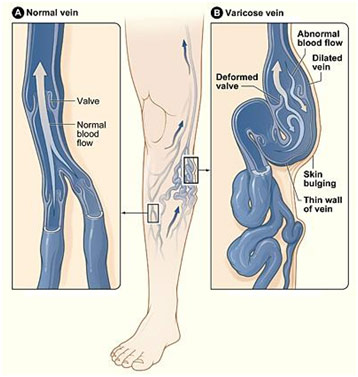
One of the first things I saw were varicose veins, which are large dilated veins that occur when the valves become incompetent and allow for backward blood flow. Most of the time, they occur in the legs, and all of the cases that I saw were patients with varicosities in the legs. Normally, veins in the legs push back blood up to the heart when we walk since the calf muscles compress them, allowing the valves to open up. However, with old age usually, these valves become weak, and this causes reflux and a resulting bulging of the vein, which can cause skin discoloration and ulcers among other things. Skin discoloration, medically known as varicose eczema or stasis dermatitis, is caused because small capillaries may rupture and leak blood into our body tissues. Fibrin, a protein that the body converts from fibrinogen in the blood, forms fibrin cuffs that surround the capillaries, causing local cell necrosis since these tissues do not get oxygen as a result. Varicose veins can cause venous ulcers as well when the disease advances because fluid coming out of the ruptured capillaries breaks down the skin. The outpatient treatment for varicose veins mainly consists of compression therapy with the regular wearing of stockings, dressing the wound frequently (if there is an ulcer), and leg elevation when lying down, which helps to improve circulation. In extreme cases where the varicose veins are not responding to therapy and affecting the patient’s quality of life, surgical therapy may be considered. However, surgery can only be done for superficial veins, which are one of two types of veins in our body with the other being deep veins. I saw quite a few varicose vein surgeries such as radiofrequency ablation and an endovenous laser ablation combined with sclerotherapy, which both have the purpose to burn the vein so that there is no reflux when the patient stands up. Both surgeries are ultrasound-guided, and both techniques cause thermal damage to the surrounding tissue. However, there are a number of differences between the two procedures. In the endovenous laser ablation combined with sclerotherapy, the surgeon often only ablates above the knee to prevent nerve damage to the nearby saphenous nerve since temperatures can reach up to 800°C. To ablate the rest of the vein, a sclerosant (foam solution where the liquid is combined with air) is inserted into the vein, which causes it to collapse. However, sclerotherapy is not usually done for the entire leg since the chance of recanalization for veins with sclerotherapy is higher than with endovenous laser ablation. In the radiofrequency ablation, the temperature is much lower as it only reaches 120°C, and it ablates the vein seven centimeters at a time. Therefore, radiofrequency ablation is preferred since it is faster and it causes less damage to the surrounding tissues.
Varicose Veins

Venous Ulcer
In addition to the varicose vein surgeries, I saw few other vascular surgeries such as Hickman Line Insertion, Chemoport Insertion, and Angioembolization of the Face. Hickman Lines are a type of “tunneled” central venous catheter for giving IV medications or taking blood draws. One of the Hickman Line insertions that I saw was to set up access for a stem cell transplant for a patient with aplastic anemia, a rare condition where the bone marrow stops producing red blood cells. The patient was under local anesthesia, and Dr. Grover used an ultrasound to find a suitable location to insert the guidewire through the puncture needle. On the wire, he put the peel-away sheath through which he introduced the catheter into the external jugular vein and then into the superior vena cava with the location being verified fluoroscopically (live x-ray). As the name suggests, the peel-away sheath simply peels away after its purpose to feed the catheter has been served. There is also a collagen-based cuff on the line that helps secure it in place and creates a barrier so that bacteria does not transmigrate from the skin. Before finishing up and suturing the Hickman Line in place, Dr. Grover made sure he was able to push in and pull out the catheter since the Hickman Line will need to be replaced if he was unable to do either. In addition, he made sure to flush the lines to make sure they do not get blocked. After seeing some Hickman Line Insertions, I saw a Chemoport Insertion on a three-month-old child with neuroblastoma, which is a tumor on the adrenal gland of the kidney. The purpose of the surgery was to make giving intravenous chemotherapy much easier. This operation was relatively simple since Dr. Grover simply made a pocket in the body to put the chemo port inside. Then, with another incision, he put the wire and catheter along with the peel-away sheath in, which is there once again to introduce the catheter. Before finishing up and closing up the incisions, Dr. Grover aspirated the catheter by drawing blood back to clear the line in order to take blood samples and to check for any small clots in the tubing, which he did not want to push further into the vessel. Lastly, Dr. Grover did an angioembolization of the face for arteriovenous malformation there since the high flow circuit would start to erode the skin without surgery. Through the femoral artery, a catheter was placed to go all the way to the facial artery. With this catheter, the surgeon injected glue (cyanoacrylate) to occlude the vessels since the glue polymerized as soon as it comes into contact with blood. Throughout the surgery, they used to contrast and fluoroscopic guidance to check their success, and before they were about to end, Dr. Grover and his team checked the internal carotid flow to make sure that none of the glue went into the internal carotid artery that feeds the brain. Dr. Grover also made it clear to me that the surgery would have to be fully accomplished over multiple sittings since it was too complex and dangerous to do it all at once.
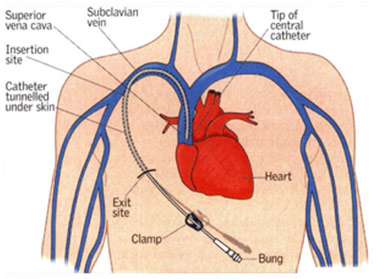
Subclavian Hickman Line Insertion
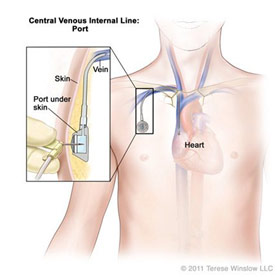
Chemo port Insertion
In addition to the vascular surgeries, I saw other surgeries from a variety of other disciplines like a kidney transplant, coronary artery bypass graft, mastectomy, and laparoscopic cholecystectomy when there were no other vascular surgery cases to see. For the kidney transplant, I only saw a little part of the harvesting process, which was done laparoscopically before the donor’s kidney was transferred to an adjacent theatre where the recipient was already under general anesthesia. The kidney transplant was quite memorable since the urology surgeon accidentally cauterized the renal artery since there was an early division into the upper polar, middle polar, and lower polar branches as it occurred before the hilum (gateway to an organ). Since the artery was supplying a good chunk of the kidney, the surgeons needed to vascularize it quickly or risk necrosis, which would have made the kidney useless. The surgeon called Dr. Grover to come in and help since he would be able to best repair the artery, which he subsequently did. Dr. Grover contemplated doing a vein graft; however, he did not see the need to since the inside of the vessel was still healthy, so it would not need to be bypassed. Therefore, he just did the primary anastomosis (sutures), making sure that he did not cause a constriction and that it would not damage the vessel. Following this complication, the urology surgeon connected the veins and arteries in the recipient’s bodies with the kidney, and he connected the kidney to the bladder. Another surgery that I saw was a coronary artery bypass graft where a cardiac surgeon harvested a venous graft from the leg to bypass the coronary artery because of coronary artery disease. There are three coronary arteries, and they may all need to be bypassed, requiring harvesting veins from both legs in some cases. In one specific case that I saw, there was a lot of fat on one of the harvested veins, so the cardiac surgeons spent time cutting the fat off, suturing any punctures that they made to the vein itself. They cut off the fat because it would become avascular and necrotic if they did not, which would increase the risk of it becoming infected. However, before they had harvested the veins, they performed a median sternotomy to gain access to the thoracic cavity and the heart. They then just stabilized one area and operated on that when it came time to graft the vessels, doing so by connecting healthy vessel to healthy vessel, bypassing the unhealthy part. In order to minimize the risks of operating on a beating heart, they had a pacing wire on the heart to electrically stimulate it if the heartbeat got too low and a defibrillator on hand as well. Following the surgery, they did the suturing and even united the sternum with a steel wire that would stay in the patient for life.
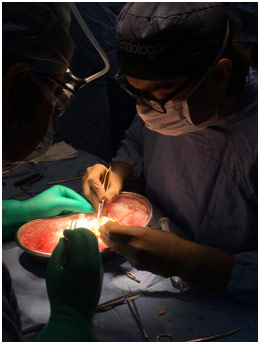
Primary Anastomosis on Kidney
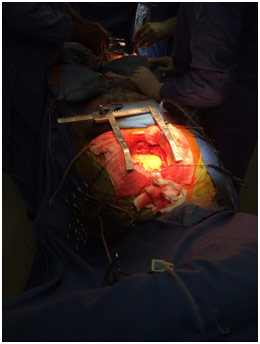
CABG with Surgeons Harvesting the Saphenous Vein
Following the CABG, I saw a mastectomy where a plastic surgeon removed the left breast of a patient who already had undergone extensive chemotherapy for her breast cancer. The surgeon made his initial incisions and began to cut the fat with the cautery, which both burns and coagulates to reduce bleeding. In addition, the surgeon made a clear point to me that he does not risk a thin flap (without much fat left on it) when doing the surgery since it can lead to flap necrosis as blood gets to the breast region through the fat. In addition to learning a little about the possible risks of the procedure, I was also able to see some of the landmarks that the surgeon used to know what to remove and what not to, like the latissimus dorsi, intercostobrachial nerve, and the axillary vein. Following the mastectomy, there were drains put in so that any fluid that accumulates would get out, and absorbable sutures were used to bring the two flaps together. Lastly, I saw a laparoscopic cholecystectomy, which is when the gallbladder is removed by a gastrointestinal surgeon, usually due to gallbladder stones. The surgery was carried out laparoscopically with only minimal incisions as the surgeon inserts a camera and operates by looking at a monitor, showing what the camera is seeing in real time. The surgeon clipped the cystic artery to keep it in place before cutting it along with the cystic duct in order to separate the gallbladder and take it out. The GI surgeon made a point here of the importance of cutting layer by layer because the anatomy is not always clear, and if the surgeon goes in without patience, they can accidentally rupture the gallbladder, spilling yellow bile while the gallbladder is still inside the patient’s body. This complication is known as biliary peritonitis and can be life-threatening to the patient. Overall, I really appreciated being able to see these various surgeries in person since it is so much different than learning the same information from a textbook for example.
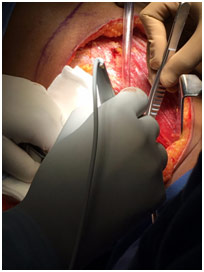
Cauterizing Following Breast Excision
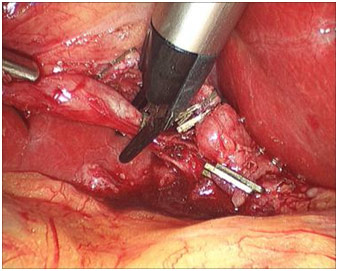
Clipping Cystic Duct and Artery
This internship was really spectacular since I was able to truly experience how a hospital works by spending ten days watching surgeries in various OTs or seeing patients in the vascular OPD. In addition, I was able to even visit the clinical meeting, which happens every Monday at Medanta, where all the doctors assemble to hear from different departments. During the time that I was there, the cardiac surgeons were presenting, and they talked about a variety of topics with one being aortic dissections. This experience was truly life-changing as I saw many things that I probably will not see again until I begin medical school in several years. In addition, I learned a lot about the Indian healthcare system, which works quite differently than the American one, and to be able to compare the two with Dr. Grover was quite fascinating. It was a privilege to be able to do an internship at Medanta, and I enjoyed every second of it.
References
Central Venous Catheter. Siteman Cancer Center, siteman.wustl.edu/glossary/cdr0000045962/. Accessed 28 Oct. 2017.
CureSearch.org. Central Venous Internal Line: Port. Riverview Cardiac Surgery, riverviewcardiacsurgery.com/thoracic-surgery/infusaport-insertion/. Accessed 28 Oct. 2017.
Laparoscopic Cholecystectomy. Placement of Clips on Distal Cystic Duct. 9 Aug. 2016. Medscape, emedicine.medscape.com/article/1582292-technique#c2. Accessed 28 Oct. 2017.
Lights, Verneda, and Lauren Reed-Guy. “Stasis Dermatitis and Ulcers.” Edited by Steven Kim. Healthline, 20 Nov. 2015, healthline.com/health/stasis-dermatitis-and-ulcers#overview1. Accessed 28 Oct. 2017.
National Heart Lung and Blood Institute. Normal Vein Vs. Varicose Vein. Medical News Today, medicalnewstoday.com/articles/240129.php#causes. Accessed 28 Oct. 2017.
“Pros & Cons.” The College of Phlebology, collegeofphlebology.com/radiofrequency-ablation/pros-cons. Accessed 28 Oct. 2017.
The Vascular System Chart. Universal Medical, universalmedicalinc.com/the-vascular-system-chart.html. Accessed 28 Oct. 2017.