Dr. Kamal Singh is a radiologist and nuclear medicine specialist, practicing in Los Angeles. He attended military medical school at the Uniformed Medical University in Bethesda, Maryland as a commissioned officer in the US Air Force. In medical school, he became interested in radiology during a clinical rotation because the aspect of combining anatomy and technology to make an impactful diagnosis was highly appealing to him. Thus, he did his radiology residency at Travis Air Force Base in California followed by a fellowship in nuclear medicine at the University of Texas at San Antonio. He appreciated this unique medical experience for many reasons, from wearing the uniform to school to becoming a soldier afterward, in large part because it allowed him to better appreciate the intricacies of practicing medicine in austere environments. In addition, this type of education allowed him to avoid excessive student loans, serve his country as he did a tour of duty in Afghanistan, and make a lifetime of memorable experiences in places and bases around the world. A few years ago, he kindly allowed me to shadow him in the radiology and nuclear medicine department at Kaiser in West Los Angeles.
Medical Imaging Scans Read by Dr. Singh
Almost everyday, I would go to one department and see how the studies were performed by observing the technologists. The first few days, I witnessed how they did a CT (Computerized Tomography) scan. The process began with bringing the patient from the waiting room and verifying their identity by checking their band. Afterward, they looked at the requisition sheet, which told them what the doctor ordered, which doctor ordered it, and why it was ordered. The patient may need IV contrast (iodine) or oral contrast (dilute barium sulfate or water-soluble gastrografin) to highlight certain structures like organs and blood vessels. The CT beam is weakened as it passes through the contrast, making it easier to recognize the region on imaging as it is colored white. Oral contrast is good for defining the gastrointestinal tract on abdomen/pelvis CT while IV contrast is good for enhancing images of blood vessels and tissues structures. Before they give the IV contrast, they have to go through a checklist of possible contraindications such as allergies. Specifically, it is really important to check if the person has kidney disease since IV contrast is cleared through the kidneys and can put someone into renal failure.
Following this verification, the patient was put on the scanner, and the technologist selected the proper protocol. The machine itself looked rather similar to an MRI machine, but it worked by rotating an x-ray machine around the patient to take a picture. The CT machine can do a total body image from head to toe extremely fast in only a few minutes, which means they are particularly useful in emergency situations. When I came back to Dr. Singh’s room, we looked at various CT scans, and he talked about how he reads them. The images are like a 3D dataset as they are spliced into different projections, which are the axial, coronal, and sagittal planes. The axial planes divide the body into horizontal sections from the bottom of the body to the top of the body. The coronal planes divide the body into vertical sections from the back of the body to the front of the body. The sagittal planes divide the body into vertical sections from the left of the body to the right of the body. Dr. Singh shifted between the different planes and images in each plane when looking at a study in order to look for clues in the images. Mostly everything in a CT scan is in shades of gray with the color being based on the density of the structure. However, Dr. Singh would periodically look specifically at a certain structure and narrow the spectrum of gray to make the distinctions clearer. However, he did not need to do this to tell bone and air apart since they are black and white respectively. With Dr. Singh, I saw cases of a cervical spine fracture from a motor vehicle accident because of a fracture line and misaligned spine as well as soft tissue swelling, avascular necrosis of the hips because of white-colored subchondral sclerosis (bone thickening in joints), and black-colored lucency (lytic lesion), and aspiration pneumonia because of a hazy density with dark lines running through it on the dependent portion of the lungs on the CT scan.
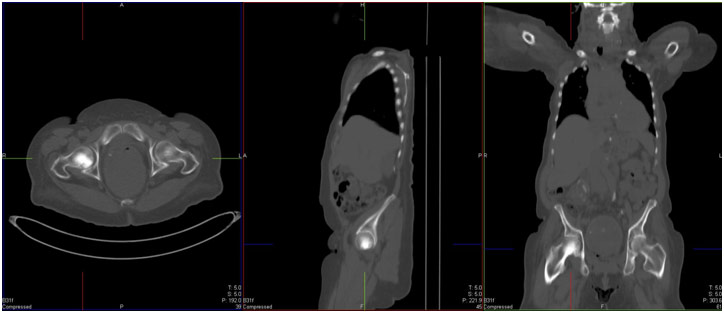
Avascular Necrosis of the Hips on CT Scan
After observing the CT technologists, I witnessed how they did an MRI (Magnetic Resonance Imaging) scan. The verification process was extraordinarily similar to the CT one with a checklist for the IV contrast (gadolinium) since it also clears through the kidneys. However, they also do additional screening for metal objects. They verify that the patient is not wearing any metal nor do they have any in them like in the form of a pacemaker, aneurysm clip, or metal shrapnel in the eye. This is because of metal moves and heats up in the MRI, which can cause internal damage. An MRI works by having a magnetic field align the hydrogen ions in our body and then by temporarily changing their direction with an electromagnetic pulse. As the hydrogen ions are getting realigned, the machine takes a snapshot. This is part of the reason why an MRI is sometimes called proton imaging.
Despite the similarities to the CT scan, I saw that an MRI was quite different for a multitude of reasons. First, there is absolutely no radiation in an MRI, and second, one MRI takes a great deal of time to complete. Just doing an MRI of a shoulder can take about thirty minutes, meaning that an MRI can only be done for certain parts of the body while a CT scan can be done for the entire body quickly. The differences do not end on the patient side also because the interpretation is also quite different for Dr. Singh. For an MRI, there needs to be a lot of different sequences, which can each take two to three minutes. For example, the GRE Gradient is used to look for blood, the T1 sequence for anatomy, the T2 sequence for physiology, DWI for acute infarct (stroke), etc. Furthermore, Dr. Singh just saw the pictures as they were, and if he wanted to see three different views, then he would have to order three different sequences. Lastly, an MRI gives much better detail for soft tissues while a CT scan gives much better detail for bones. With Dr. Singh, I saw a case of acute cerebral infarct because of the restricted diffusion of water on the DWI (diffusion-weighted imaging) sequence, multiple sclerosis because of bright spots in the white matter around the ventricles, and glioblastoma multiforme because of a vague mass that has greatly infiltrative features on the MRI scan.
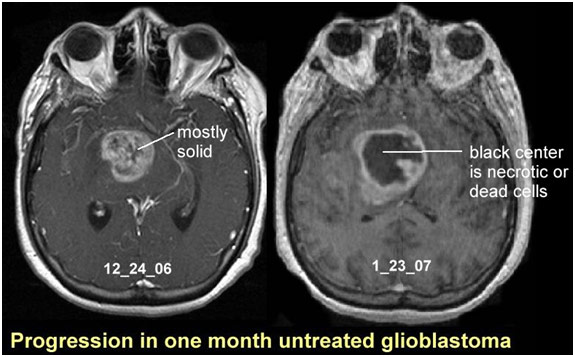
Glioblastoma Multiforme’s Rapid Progression on MRI
The following few days I accompanied the Ultrasound and X-Ray technologists. The ultrasound exams were very hands-on with the patient as the technologist was holding the probe and moving it across the patient’s skin after putting some ultrasound gel on it. It works by sending sound waves that show different tissues based on how the waves get reflected back to the receiver. The technologist can also turn on color, which is to show blood flow. The colors themselves do not matter since they can be switched by just rotating the probe, but they represent blood flowing towards the probe and blood flowing away from the probe. Since there is no radiation involved, there is little to no screening involved on the patient-side. However, unlike a CT scan, you cannot do an ultrasound of the entire body as it is very labor-intensive. The technologist has to take a picture and save it with a caption each time, and it can take up to fifteen minutes. With Dr. Singh, I looked at some ultrasounds and talked to him about what we were seeing. The main thing about ultrasounds is that they are hard to read since the anatomy is not especially clear. Dr. Singh often had to rely on the technologist to tell him what is going on. Part of the problem is also that the taken pictures are still, but Dr. Singh needed to know what was happening between the times the pictures were taken. I saw an ultrasound from the hip to knee, looking for a blood clot in the leg (deep vein thrombosis). There were only twenty photos that Dr. Singh received; however, he very well could have also received a million if he got a snapshot of every single moment during the scan. Thus, the technologists needs to be very good at what they do and know exactly what they are looking for to better assist the radiologist in analyzing the ultrasound exam. The radiologist also relies heavily on a good history since many conditions mimic others. For example, an abnormal liver on an ultrasound can be the result of a tumor, infection, trauma, or severe inflammation. It can also just be congenital. With a good history, the radiologist can narrow it down to a few or even just one, making the diagnosis better. In one case, the ultrasound looked like there was a tumor, but after finding out that the patient got punched in the gut a few days before, Dr. Singh told me that it was probably internal bleeding due to trauma. Because of the problems described above, doctors end up relying on a CT scan or MRI to give them more information, but ultrasound is useful in getting relatively good information fast.
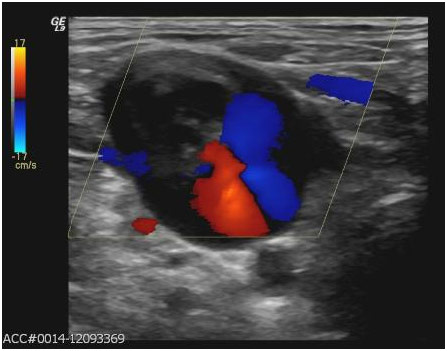
Deep Vein Thrombosis on Ultrasound
Following this experience with the ultrasound technologists, I visited the x-ray technologists. An x-ray is extraordinarily simple, and a technologist described it to me as being the bread and butter of radiology. The patient either stands in front of a machine or lies down on a bed with the machine above them, and the machine quickly takes a 2D picture. I also learned more about radiation safety because I always had to be outside of the room, behind a lead window, or wearing a lead apron when an x-ray (and a CT scan) was in progress since the x-ray ionization radiation can be harmful by causing mutations in our DNA. Like the ultrasound, there was not much screening except for large metal objects since the x-ray cannot go through metal. With Dr. Singh, I saw him diagnose tuberculosis because of cavitation in the upper lung, a hip fracture in a patient who fell down due to a saw fracture line indicating a broken femoral neck, and rheumatoid arthritis on a foot x-ray due to erosions along the joint that looked punched out.

Rheumatoid Arthritis Erosions on X-Ray
After those days, I was able to observe how the PET/CT scan was done. It uses a dual mechanism that has both PET and CT scanning capabilities built into it. The technologist injects a radiopharmaceutical, often radioactive glucose into the body in order to look for cancer. Cancer uses glucose metabolism to multiply since the cells are dividing, so they use glucose to make ATP for energy. Places that show up as bright often indicate cancer since cancer uses up more glucose than normal tissue. A PET/CT scan can take a scan of the whole body, and it can be used to differentiate between different stages of cancer and to find cancer in its earliest stages where a CT scan or MRI might miss it. Dr. Singh also told me that a PET/CT scan can be used to see if the cycles of chemotherapy are working or not by seeing how much dead tissue (tumorous cells that responded to chemotherapy) is present since dead tissue does not do any metabolism (take up any glucose). Before, determining the patient’s response to chemotherapy was all based on the size as radiologists thought that if the tumor got smaller, then the chemotherapy is working. They would check up after three months and look if the tumor stayed the same or got bigger, which it did from time to time. If the tumor did get bigger, the radiologist realized that they needed to add drugs or start the chemotherapy up again, which would have been better to have done before. Thus, the PET/CT scan has completely revolutionized the way we treat cancer by seeing if the therapy is really working or not. With Dr. Singh, I saw him diagnose diffuse large B-cell lymphoma (cancer of lymph nodes and bone marrow) as there were diffusely enlarged lymph nodes above and below the diaphragm with intense bright spots on PET, small cell carcinoma as there was a central lung mass with mediastinal and hilar adenopathy (lymph node swelling) with again intense uptake on PET, and osteosarcoma (bone cancer) in the femur because of a large sclerotic bone mass that extended into the soft tissue and was brightly colored on PET. In regards to the lung cancer case, I also attended a multidisciplinary conference with various other medical professionals such as a pulmonologist, thoracic surgeon, and oncologist. Basically, one doctor presented the case, showing pictures, and having a discussion with the other doctors like Dr. SIngh. In this specific case, the small cell carcinoma was only in the lungs and mediastinum and had not metastasized to the other places. Thus, the thoracic surgeon said that he can take it out, and Dr. Singh warned that the patient will likely need radiation therapy afterward.
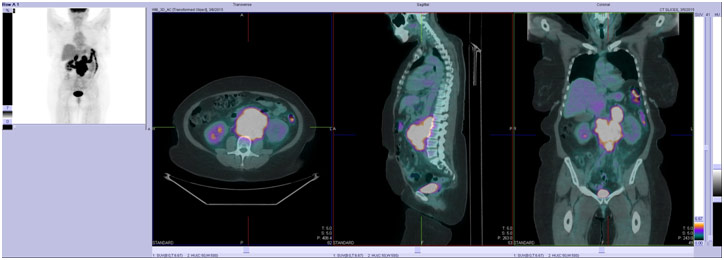
Diffuse Large B-Cell Lymphoma on PET/CT Scan
Lastly, I went to see how nuclear medicine was done. Nuclear medicine is quite different than radiology as it involves putting radiation, through an injection or oral administration based on what the radiologist is trying to get a picture of, in the body. The basis of nuclear medicine is the radiopharmaceutical, which is the combination of a radioisotope, which decays and emits photons (gamma waves) that can be picked up by certain detectors to form an image, with a pharmaceutical, which takes the radioisotope to the organ and helps us determine that specific physiology. For imaging the biliary system, for example, the radioisotope Technetium is labeled to the pharmaceutical HIDA, which is taken up by the liver and is actively secreted into the bile ducts, in order to determine if the gallbladder is obstructed with gallstones for instance. However, this means that nuclear medicine can take really long like between 2-6 hours. For a bone scan, the tech injected the radiation and told the patient to come back in 3 hours. Then, for 30-40 minutes, she was taking the pictures. The machine takes about 2-5 minutes to create, collect, and save each image; it can also make a movie as well. The tech emphasized the need for precision here because the radioisotope not only affects the organ targeted but everything next to it as well, which really raises the stakes. When Dr. Singh showed me the images and short movies, I was taken aback because I thought ultrasound was difficult to understand, but nuclear medicine was even harder. There was really no anatomy to help orient me, so it was difficult to put the image or movie into perspective. However, it was special to see human physiology as it happened. With a myocardial perfusion scan (MPS) in the case of ischemia (lack of blood to the heart) due to coronary artery disease, I saw that there was no issue with the image of the left ventricle in the resting state, but after treadmill stress, there was decreased counts of radiotracer activity in the left ventricular wall, indicative of decreased perfusion. I also was able to see a gastric emptying study in order to see if the patient is gastroparesis or slow emptying of food from the stomach, which can cause symptoms of bloating and nausea in diabetic patients. In the study, the patient ate radioactive eggs with Technetium and a sulfur colloid that attaches to the protein in the eggs. It should have taken only 4 hours for the stomach to empty the food, but it took much longer for the diabetic patient. Lastly, I also saw a thyroid ablation for extreme cases of hyperthyroidism because hypothyroidism, which would be caused by the ablation, is a much safer and more manageable disease to have. The patient was put in a special room with lead walls and given pills containing radioactive iodine (I-131) that are absorbed in the blood. Through sodium-iodine symporters, the I-131 gets into the thyroid and kills the cells through the emitted high energy, low-range photons.
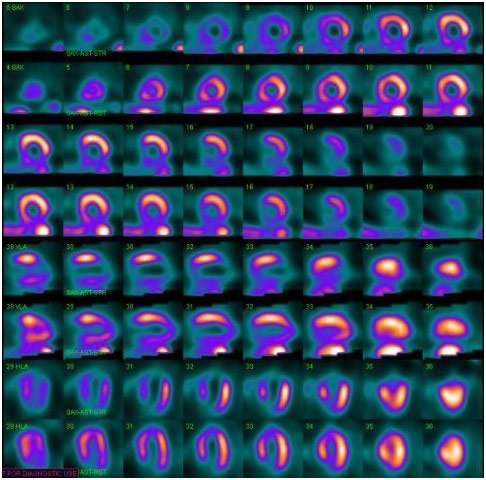
Myocardial Perfusion Scan in the Case of Ischemia
This shadowing opportunity was done before I even started this medical blog, and I only recently found the notebook in which all my notes were kept. I remember it being such a great insight into the life of a radiologist as well as a nuclear medicine physician as well as a great way to meet patients and try to understand their symptoms for which they were getting images done. Sometimes, it was just to confirm a diagnosis while other times, the medical team truly had no clue and was requesting the image to help give them more insight. It was such a privilege to be able to shadow Dr. Singh at such an early time for so long, and I truly enjoyed every part of my experience, from spending time with the techs to interpreting the images with Dr. Singh to reveal the story in the patient’s body.
References
“Information about Intravenous and Oral Contrast Used in CT.” Imaginis, www.imaginis.com/ct-scan/information-about-intravenous-and-oral-contrast-used-in-ct-1. Accessed 11 Apr. 2019.
Progression in One Month Untreated Glioblastoma. About Cancer, www.aboutcancer.com/mri_gbm.htm. Accessed 11 Apr. 2019.
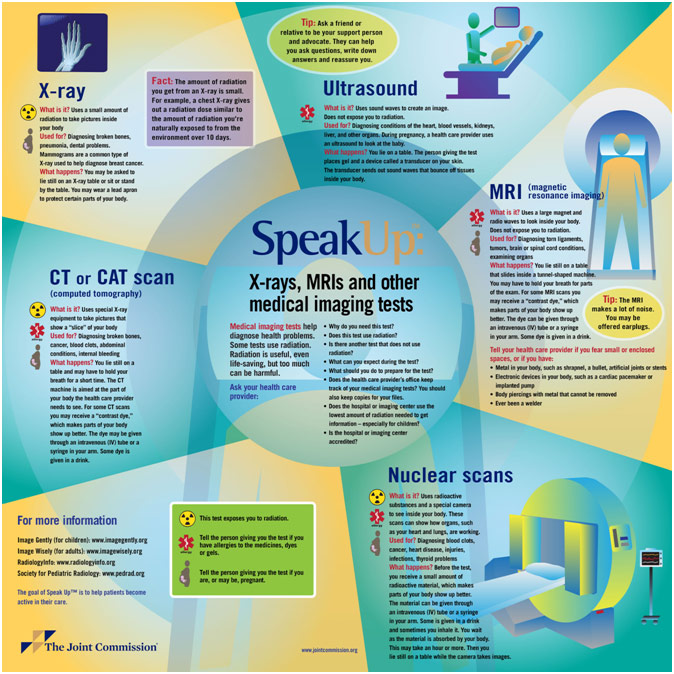
Speak Up Infographic. The Joint Commission, jointcommission.new-media-release.com/2014_su_medical_imaging/. Accessed 11 Apr. 2019.