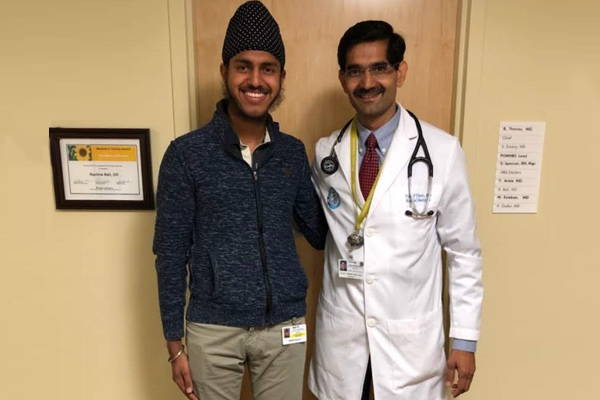
Dr. Vijay Tiwari is an internal medicine specialist, or internist, practicing in San Leandro with Kaiser Permanente. He attended Government Medical College in Trivandrum, Kerala, India. He then moved to the US where he did his internal medicine residency at San Joaquin General Hospital in California. He chose the field of internal medicine because he liked being able to get into the details of the patient’s history and being able to save their life, or greatly improve their quality of life, treating the patient’s story. In his words, the more accurate a story he gets from the patient, the more accurate the treatment will be. That detective-like work greatly appealed to Dr. Tiwari and is where his passion for medicine comes from. Dr. Tiwari is also a truly remarkable man, overcoming numerous difficulties that afflicted him when he was young. He grew up in poverty in a small Indian village, living on one meal a day and drinking water to stay full. He is such an inspiring person because he, nevertheless, did the seemingly impossible, coming to the US and becoming a top physician at Kaiser who has risen to positions like associate chief of the hospital before choosing to step down to go back to treating patients.
Dr. Tiwari first explained to me the basics of Kaiser. Kaiser is a Health Maintenance Organization (HMO) while most other hospitals are Prefered Provider Organizations (PPO). Kaiser has a vested interest in keeping their patients healthy because they pay them the same amount (monthly premium) whether they are healthy or sick since there are small to no deductibles that a patient has to pay at HMOs. They make more money when you stay healthy than when you are sick. PPOs, on the other hand, make money when the patient is sick since they tend to have high deductibles that the patient has to pay every time they see a doctor. I found this as a very interesting distinction that I had not thought about before. Even more interesting was the fact that Kaiser is made up of three separate companies—Kaiser Foundation Hospitals, Kaiser Permanente Health Plan, and The Permanente Medical Group. The Kaiser Foundation Hospitals own all the building, equipment, and employ some of the nursing staff. It is a non-profit. The Kaiser Permanente Health Plan is the insurance company that sells the product and provides a network of doctors for its members. It is a nonprofit. The Permanente Medical Group is a group of doctors and clinicians who have exclusive contracts with Kaiser Foundation Hospitals and Kaiser Permanente Health Plan members. They, on the other hand, are for profit.
In regards to the medical structure of the Kaiser hospitals, there are four levels of care for someone who comes in with an urgent need—Emergency Department, Med Surg, Med Tele, and ICU. The Emergency Department (ED) is where the emergency room physicians determine if the patient should be discharged, observed, or is sick enough to be seen by a specialist like Dr. Tiwari. They are then put in the clinical decision-making area (CDA) in the ED where the internist makes an assessment of whether to admit them to the hospital or keep them in the ED. If admitted, they usually go first to the Med Surg level where the patient is under direct observation without any monitoring. If they are in critical condition, they may also go to the Med Tele level where health care professionals are watching their heart rate 24/7 among other monitoring of their vitals. The highest level of care is in the Intensive Care Unit (ICU), which also has constant monitoring but has more frequent documentation of this monitoring. For example, labs can be taken as frequently as every one hour in the ICU contrasted with every four hours in Med Tele. The ICU also has a much smaller nurse to patient ratio since it is usually 1:1 to 1:2 contrasted to the 1:4 to 1:5 of Med Tele.

Intensive Care Unit (ICU)
There was a multitude of patients that we saw in all four levels of the hospital. A few of them especially demonstrate the difficulty of Dr. Tiwari’s job though. One patient came into the ED after suffering from a fall due to a syncope episode (fainting). However, this patient also had other coexisting disorders like chronic heart failure (heart function impaired), atrial fibrillation (irregular beating of the heart), hypertension (high blood pressure), dyslipidemia (all types of variance in cholesterol), and diabetes (high blood glucose). Dr. Tiwari read the chart and reviewed this problem list before going in to see the patient. He then confirmed the history with the patient and did his own assessment, using his stethoscope to auscultate for example. After talking some with the patient, Dr. Tiwari went to reconcile their medications, determining which medications the patient should continue to take and which ones they should not. For example, doctors never give metformin, a diabetes medication, in the hospital setting, instead of using an insulin sliding scale. This is because metformin is excreted through the kidneys and if the patient is given IV contrast, a common step in imaging, the kidneys will be destroyed. Dr. Tiwari then ordered some tests to try to determine the cause of this patient’s syncope. He told me that it could either be caused by the brain, the heart, dehydration, or low blood sugar. The CT scan came back normal, the blood sugar was found to be normal, and the patient had normal creatinine, which indicated the patient was not dehydrated. Thus, Dr. Tiwari kept this patient in Med Tele until myocardial infarction (MI) could be ruled out or be confirmed as the cause of the patient’s syncope. He then documented this whole instance, telling me that if patient interaction isn’t documented, it didn’t happen.
Another patient interaction was particularly interesting. A patient came into the ED with hyperglycemia with blood sugar in the 800s. Dr. Tiwari urgently needed to see him because he told me that this patient could have diabetic ketoacidosis as the lab work showed his ketone to be positive. Diabetic ketoacidosis (DKA) is a potentially fatal condition characterized by high acidity in the bloodstream due to the breakdown of fatty acids since glucose cannot be effectively stored and used. Since all drugs are designed to be most efficacious between normal blood pH of 7.35 and 7.45 and our body’s enzymes can undergo pH inactivation at different levels of pH, restoring the patient’s pH to normal levels was paramount. The patient was quickly moved to the ICU where the patient was given an insulin drip with the goal of bringing the blood sugar below 250. This would help reduce the blood acidity by driving the acidic ions from the blood into the cells. The nurses also started loading him up with IV fluid for two reasons. The first was to dilute the blood to also reduce the acidity, and the second was to reduce the risk of the patient going into a coma caused by the low blood supply to the brain. The lab work also showed that the patient had hyponatremia (low sodium levels), making this seem like an endlessly complicated case; however, Dr. Tiwari said that it was actually pseudo hyponatremia because this low sodium level was caused by the patient’s high blood sugar, not something else. Sodium was pushed out of the viscous blood and into the cells due to the principle of osmosis. For every 100 units rise of blood glucose, there needed to be a correction of 1.6 units of sodium to treat this pseudo hyponatremia. This high-intensity case gave a glimpse into the everyday fast-paced job of Dr. Tiwari.
Urinary Tract Infections (UTI) often are the cause of a patient’s admission to the emergency department. There were quite a few patients with UTI or suspected UTI, but some were more unforgettable than others. In one example, Dr. Tiwari saw a patient who presented with delirium (extreme confusion). Initially, Dr. Tiwari’s mind went to UTI as the cause of confusion since that is the most common cause of confusion in the elderly. However, after taking a full history, Dr. Tiwari found out from the patient’s family that the patient has been in a dementia facility for the past three months. Dr. Tiwari decided to thus keep a sitter and observe the patient overnight while also ordering labs for the patient’s urine culture. Specifically, the labs look if nitrates and esterase are positive since both are made by bacteria in the urine and would indicate the patient has an infection. The labs will also show an elevated white blood cell count if the patient has a UTI since the body has started to fight the infection. Not wanting to wait for the labs to come back, Dr. Tiwari preemptively started 24 hours IV antibiotics, which he would continue or end based on the patient’s condition. All of these clinical examples helped me see that doctors are like detectives. They must systematically look through potential causes for the patient’s ailment and rule them out one by one in order to help patients get better.
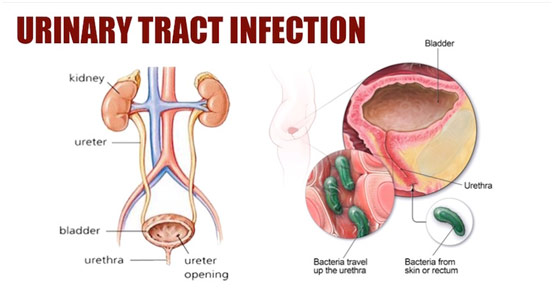
Urinary Tract Infection
Because the emergency department can have such an irregular flow of patients, Dr. Tiwari sometimes had long breaks. There we talked more specifically about some aspects of the hospital system and care. For example, he explained to me what the four parts of a clinical note, the norm for documentation, are. They can be remembered through the acronym SOAP (Subjective, Objective, Assessment, and Plan). The subjective portion includes what the doctor sees upon first glance and what the patient reports have happened, which includes when/how the injury occurred and the severity of the chief complaint among other things. For example, the patient may say they have a terrible fever and say they are coughing a lot of phlegm. The objective portion regards what the doctor finds after doing some lab testing and checking the vital signs. For example, upon auscultation, the doctor may hear crackles and find a slight fever. The assessment is about what the doctor thinks is the diagnosis, made with the help of the subjective and objective portions. For example, it would be pneumonia in this case, which can be tested by taking a sample from their cough by inducing a sputum. The plan would be what the doctors want to do in regards to the treatment plan or hospital level plan. For example, the doctor may start broad antibiotics, wait for the patient’s blood culture, and follow up with the results by narrowing down the antibiotics. The blood culture can help determine what kind of infection there is based on the percentages of the five components of the white blood cells, which are neutrophils, lymphocytes, monocytes, eosinophils, and basophils (no longer monkeys eat bananas). Generally, bacterial pneumonia means neutrophils are predominant (neutrophilia); viral pneumonia means lymphocytes are predominant (lymphocytosis); drug fever, which is when a drug causes a reaction that mimics an infection, means monocytes are predominant (monocytosis), and a parasitic disease means either basophil are predominant (basophilia) or eosinophils are predominant (eosinophilia).
Dr. Tiwari also told me about some of the most common labs that he orders to help him make a diagnosis. The basis is ionic disarrangement. One of the first important ions is potassium, a channel that is ligated by magnesium, which simply means the potassium channels will not open if magnesium is not repleted in the body. Since potassium is important for the function of muscles like the heart, low potassium (hypokalemia), usually caused by low magnesium, as well as high potassium (hyperkalemia), usually caused by excessive potassium supplements or inability of kidneys to excrete potassium, can cause arrhythmias, which is simply an irregular heartbeat. For hyperkalemia, the heart arrests when it is dilated (systole), and for hypokalemia, the heart arrests when it is contracted (diastole). Sodium is the next important ion since it plays a crucial role in brain function and nerve transmission. If sodium is too high (hypernatremia), common symptoms are confusion and lethargy. If sodium is too low (hyponatremia), common symptoms include confusion and headaches along with seizures. Another important ion is calcium since it is related to muscle weakness. If calcium is too high (hypercalcemia), common symptoms include muscle weakness and paralyzation. If calcium is too low (hypocalcemia), common symptoms include muscular spasms and hyperactive nerves/reflexes. The last important ion is bicarbonate, but it is different from the rest since having too high or too low bicarbonate is not usually a problem. Instead, bicarbonate along with blood pH and pCO2 helps make a diagnosis. They help determine if the patient has respiratory acidosis/alkalosis or metabolic acidosis/alkalosis. Acidosis and alkalosis can be caused by a problem in the lungs, the kidneys, or both. For example, a patient may have COPD (chronic obstructive pulmonary disease), which causes them to retain lot of carbon dioxide, which when mixed with water makes carbonic acid, which can cause pulmonary acidosis. Another example may be, due to decreased kidney function, the patient is not producing enough bicarbonate, which is basic, to account for the acidification of the blood, which can cause metabolic acidosis. Each mechanism can try to compensate for the other though, but the solution is not long term. A patient with primary metabolic acidosis will start to breathe harder and faster to get CO2 out of the lungs, so the patient will also have secondary pulmonary alkalosis. A patient with primary respiratory acidosis will have their kidneys release a lot of bicarb to reduce the blood acidity, so the patient has secondary metabolic alkalosis. Either coping mechanism is not sustainable though and can cause complications like respiratory failure, which is why urgent intervention by the doctor is paramount.
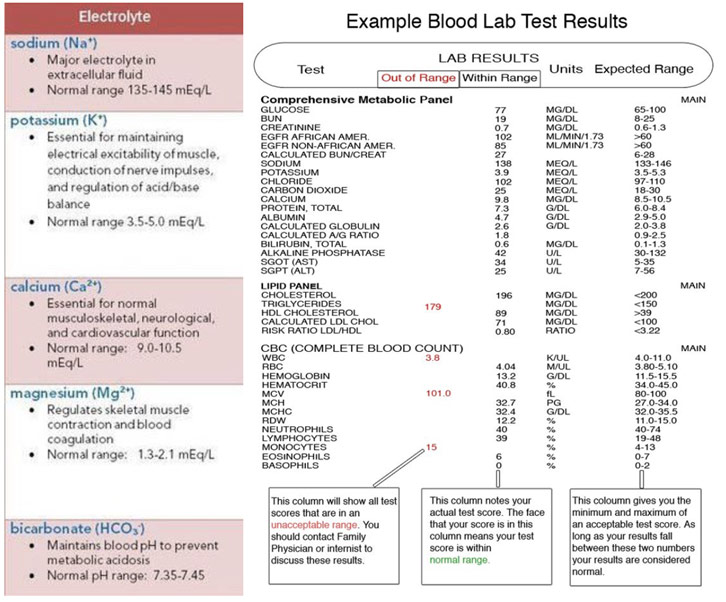
Normal Values of Five Electrolytes Along with Sample Blood Lab Test
In the last few days, Dr. Tiwari and I spent time in the Perioperative Medicine (POM) clinic. Basically, a patient comes in with a problem that requires surgical correction, so an internist sees them in advance to risk stratify and avoid any potential complication of the surgery. This department is so important because to prevent all complications is to save $3885 (cost of an ICU bed per day) times the number of days the patient is in the ICU. One of the biggest tools the POM Clinic uses is the Gupta Risk Calculator, which uses the patient’s age, creatinine level (a waste product that passes through kidneys), ASA class (classification for medical fitness), preoperative functional status (physical fitness), and the type of surgery (procedure site) to determine percent mortality. Anything about 1% is high, and anything above 4% is especially high. Before meeting the patient, Dr. Tiwari looked at the patient’s labs, their current medications, their most recent imaging, their cardiology examination results (EKG, myocardial perfusion, cardiac stress test), previous surgery history, and family chart. He then calculated the Gupta Risk Score and met with the patient. There he asked them specific questions like if they have had any previous difficulty with anesthesia if they use a breathing machine/inhaler, what their functional capacity is if they have a cardiac stent and if they are okay with blood transfusion. If they have used a breathing machine or inhaler recently, Dr. Tiwari wanted them to continue using it on the days leading up to the surgery since they are dependent on it, and not using could cause bronchospasms (lung tissue withdrawing) during surgery. If they had a cardiac stent put into place, then Dr. Tiwari could not tell them to stop aspirin-like he does for most other patients because he does not want the patient to get a blood clot. Lastly, he asked if they are okay with blood transfusion since certain religions like Jehovah’s Witnesses are not. After looking over all other relevant data, like potential pregnancies, and reviewing all of their systems to ensure no other condition will interfere with the surgery, Dr. Tiwari sent them out with a note. This note told them to stop all herbal supplements and vitamins, to stop taking all blood thinners (use Tylenol for pain instead of ibuprofen), to only eat/drink a certain number of hours before the surgery, to take specific medications the morning of the surgery that will not be contraindicated, and lastly to not smoke since smoking makes recovery significantly slower. We saw patient with surgeries like bilateral total knee arthroplasty for osteoarthritis (replacing the knees), bunionectomy (removal of a bony growth), thyroidectomy for a goiter compressing the carotid artery (removal of the thyroid), herniorrhaphy (repair of bulging organs/tissues), and panniculectomy after a great deal of weight loss (removal of hanging fat).
https://www.youtube.com/watch?v=BA6ZUsf5jdo
Video on Perioperative Medicine
On the first day I came into shadow, Dr. Tiwari told me I should try to develop a vision and then march wholeheartedly towards that. A vision in medicine, though, should not only include your future specialty but also the love for humanity that is so paramount for doctors. Dr. Tiwari taught me a lot about medicine, but he taught me more about being human. Even when rounding at 1:00 AM, he was cheerful, always making his patients smile because, in his words, nobody comes to the hospital happy and one small joke can really change people’s mood and lift their spirits. He taught me what it is like for a person to truly enjoy their work and devote themselves 100% to that end as I witnessed him go above and beyond what the job required of him. He taught me that anything is possible by recounting his own life story where he went from a boy stuck in poverty in a rural Indian village to the associate chief of an enormous well-known hospital in the Silicon Valley. He has inspired me to strive for greatness and never lose hope, no matter how bleak the situation may seem. Thank you, Dr. Tiwari.













Your logic unnerves me …