Several months back, I took a Northwestern CME Course on breast cancer screening and prevention that gave me insight into this devastating disease, the most common type of cancer in women worldwide. In 2018, the Breast Cancer Research Foundation estimated that nearly 270,000 cases of breast cancer were diagnosed in the US. On average, women in the US face a lifetime risk of developing breast cancer of about 12%, but this risk is not spread out uniformly with jumps in risk coming with old age. The guidelines around screening are set to try to catch breast cancer in its earliest stage in order to best improve outcomes while also avoiding unnecessary care with its extra radiation exposure and burden on healthcare costs. Understanding screening and prevention thus takes on special importance in order to adequately deal with this widely prevalent, devastating malignancy.
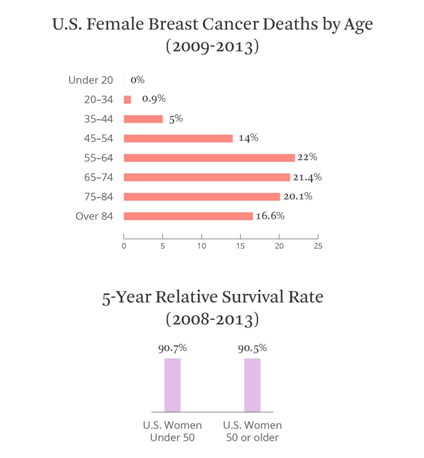
Breast Cancer Deaths by Age
A screening mammography is the most common type of imaging for breast cancer there is. The sensitivity, how often a test finds a genuine positive result, of screening mammography ranges from 77-95%. The specificity, how often a test finds a genuine negative result, ranges from 94-97%. Screening mammography works by doing a low radiation x-ray of the breasts, which are flattened by two plates, in the search of subtle differences in shape and density of the breast parenchyma, or functional tissue. With every screening mammography, the radiologist gets four images, two cranial-caudal (top-down) and two mediolateral obliques (side-side) to look for abnormal edges (speculations), suspicious calcifications, etc. Generally, starting at 40 and continuing at annual or biennial intervals, women get screening mammography, but doctors may choose to start earlier if the patient has a higher risk of developing breast cancer. The breast cancer mortality risk reduction associated with mammography typically increases with age, but for women from 40-74, the average risk reduction is 15-20%, making screening mammography an important screening mechanism.
However, like with all screening, there are certain costs that must be weighed. In fact, the chance of obtaining at least one false-positive result from screening mammography is more than 50% after 10 years of annual screening. False positives can be quite devastating by causing the patient misplaced stress and anxiety. Perhaps worse is the overdiagnosis of breast cancer. A small tumor that might never become malignant or even symptomatic is often unnecessarily treated, causing the complications of chemotherapy or surgery for no apparent benefit. In fact, the aggressive diagnosis and treatment of ductal carcinoma in situ (DCIS), a type of breast cancer that only progresses in 30-50% of cases, has not led to any reduction in the number of invasive breast cancer cases. To effectively treat breast cancer means finding the sweet spot between undertreatment and overtreatment to ensure the best outcomes for patients.
Screening Mammography Study
Other forms of imaging include ultrasonography, MRI, and tomosynthesis. Ultrasonography uses sound waves to image the breasts, specifically for patients with denser breasts. While quite low-cost, ultrasonography’s benefits have come into question. For every 1000 cases, 1.6-4.3 more malignancies are found, but there are many false positives: less than 10% of subsequent biopsies indicate breast cancer. An MRI is generally reserved for patients with an increased lifetime risk of developing breast cancer (≥20%). While an MRI is quite sensitive, it is not especially specific, so there is a high incidence of false positives associated with a breast MRI. In fact, breast MRIs increase callbacks and biopsies by three to five times. A tomosynthesis, or 3D mammography, is another supplement to screening mammography as it can allow for better identification of possible tumors in the breast parenchyma as the radiologist can more easily see around the edges. When compared to screening mammography, tomosynthesis has been shown to increase breast cancer detection and reduce false-positive rates, making tomosynthesis quite promising as a screening mechanism.
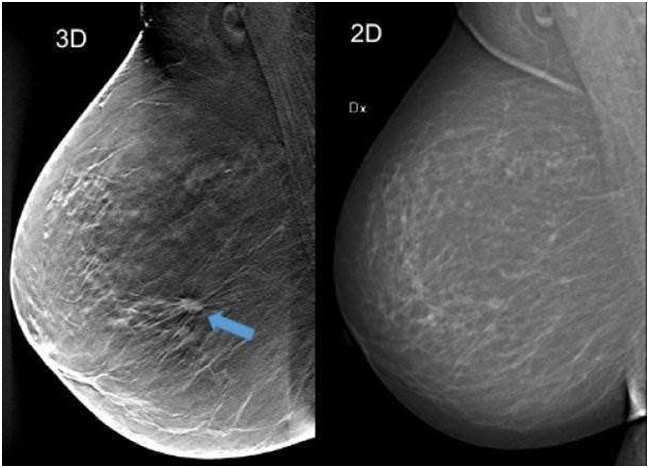
Tomosynthesis (3D) vs. Screening Mammography (2D)
Properly screening breast cancer is good, but preventing breast cancer in the first place is even better. First, it is paramount to understand the risk factors for breast cancer, both nonmodifiable and modifiable. Gender, for instance, is an important nonmodifiable risk factor: women are about a hundred times more likely to get breast cancer than men, largely because of men’s low levels of estrogen and inactive breast tissue. Age is yet another paramount risk factor as 70-year-old women are ten times more likely to develop breast cancer than 30-year-old women. White women are the most likely to develop breast cancer, making race an important risk factor as well. Of course, genetics is one of the most famous nonmodifiable risk factors as the mutations in the BRCA 1 and BRCA 2 genes increase the chance of a woman developing breast cancer from 12% to 70% by preventing proper DNA. Mutations in other genes like PTEN, p53, and PALB2 also predispose a patient to breast cancer. Nevertheless, genetic testing is generally only recommended for patients diagnosed with breast cancer when they were younger than 50 and patients with a family history of one of these mutations.
Surplus estrogen exposure can be both a nonmodifiable and modifiable risk factor as an estrogen has been thought to promote the fast growth of breast cells, increasing the chance of a random error during mitosis and thus the chance of a tumor. For instance, women who face early menarche (menstruation) or late menopause have higher nonmodifiable estrogen exposure. However, often used to treat menopause symptoms, hormone replacement therapy, specifically estrogen and progesterone combined, has been shown to increase breast cancer risk significantly. Another modifiable risk factor is obesity as the increased fat results in increased estrogen levels. Consuming alcohol and smoking have also been demonstrated to increase breast cancer risk with the former doing so by reducing the liver’s ability to metabolize estrogen, thus increasing estrogen levels. However, this mechanism is still not well understood with some believing that alcohol actually results in the aromatization, and thus production, of additional estrogen. Others believe that the cause is something else entirely.
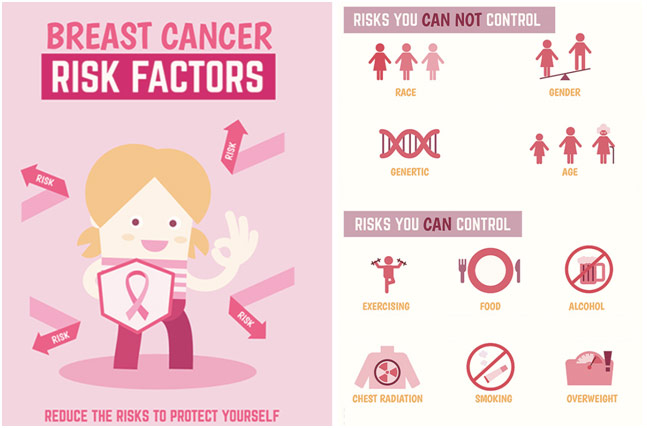
Breast Cancer Risk Factors
Prevention for breast cancer usually falls into three buckets: lifestyle modifications, risk-reducing medication, and risk-reducing surgical intervention. In regards to lifestyle modifications, staying active, avoiding alcohol and smoking, eating healthy, and maintaining a healthy weight go a long way in reducing the risk of breast cancer, especially considering that only 5-10% of breast cancer cases are caused by genetics. While the birth control pill has been shown to slightly increase the risk of breast cancer, the benefits far outweigh the risk. Furthermore, having an abortion, wearing a bra, and using deodorant have all been shown to NOT increase the risk of breast cancer. For patients with moderate to high risk of developing breast cancer, medication like tamoxifen, raloxifene, and aromatase inhibitors can be used to reduce the risk. Tamoxifen is the primary one prescribed and works by competing for estrogen’s receptors so that the estrogen cannot bind and signal breast cells to grow; tamoxifen has been shown to reduce the incidence of invasive breast cancers by nearly 40%. A selective estrogen receptor modulator as well, raloxifene works similarly. Aromatase inhibitors, mostly given to postmenopausal women, work by preventing the enzyme aromatase from converting androstenedione and testosterone into estrogen. Arimidex and Aromasin, two examples of aromatase inhibitors, have been shown to decreases the risk of developing breast cancer by over 50%. Lastly, surgical risk reduction for breast cancer involves a prophylactic mastectomy, elective preventative removal of one or both breasts. With a 90% breast cancer risk reduction, a prophylactic mastectomy seems like it would be enormously beneficial, but some studies have demonstrated no survival benefit because of surgical complications among other things. While all efforts should be made towards preventing breast cancer, the risk reduction must always be balanced with the risk of side effects.
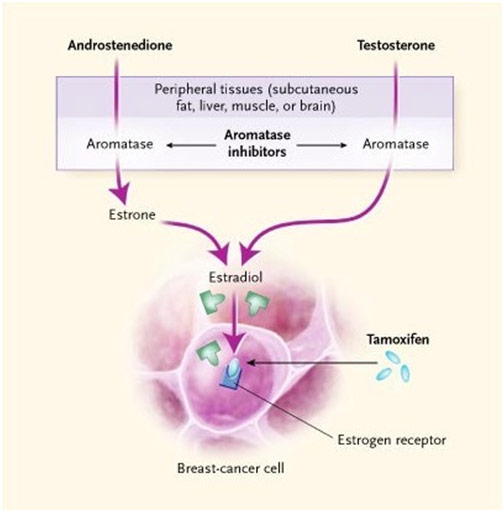
Mechanisms of Action for Aromatase Inhibitors and Tamoxifen
Breast cancer screening and prevention are among the best for all cancers, and it truly does improve outcomes for this devastating disease. In large part, breast cancer screening and prevention has come so far because breast cancer is the most funded cancer out there, period. Funding often comes from awareness, and awareness for breast cancer is stellar. We should be taking lessons from the success of breast cancer research and working to apply it to other important diseases to improve patient outcomes across the board. For instance, the rallying of the breast cancer community behind the easily recognizable and visible symbol of a pink ribbon proved vital to increasing breast cancer awareness. Breast cancer advocates enlisting the support of companies that wanted to show customers they were socially conscious, while controversial because of disease commercialization concerns, fundamentally improved breast cancer awareness. Most importantly, however, breast cancer patients are terrific advocates for themselves, making sure lawmakers truly understand the devastating impact of breast cancer. They bring great awareness and thus funding to their cause by speaking up. At the end of the day, only when patients become strong advocates for themselves and their diseases is a true change made. That is the primary translatable lesson from breast cancer.
REFERENCES
“Accuracy of Mammograms.” Susan G. Komen, ww5.komen.org/BreastCancer/AccuracyofMammograms.html. Accessed 8 July 2019.
Aromatase Inhibitors in Breast Cancer. New England Journal of Medicine, www.nejm.org/doi/full/10.1056/NEJMra023246. Accessed 8 July 2019.
“Being a Woman.” BreastCancer.org, www.breastcancer.org/risk/factors/woman. Accessed 8 July 2019.
Breast Cancer Risk Factors Infographic. 123RF, www.123rf.com/photo_43549276_stock-vector-breast-cancer-risk-factors-infographics-health-care-and-medical-information.html. Accessed 8 July 2019.
“Breast Cancer Statistics & Resources.” Breast Cancer Research Foundation, www.bcrf.org/breast-cancer-statistics-and-resources. Accessed 8 July 2019.
“Factors That Do Not Increase Breast Cancer Risk.” Susan G. Komen, ww5.komen.org/BreastCancer/FactorsThatDoNotIncreaseRisk.html. Accessed 15 July 2019.
Infographic: Breast Cancer. Alliance Cancer Center, www.alliance-greenville-clarksdale.com/news/infographic-breast-cancer/. Accessed 8 July 2019.
Kulkarni, Swati. “Breast Cancer Screening and Prevention.” IMS Webcast, 23 Sept. 2015, imswebcast.feinberg.northwestern.edu/Mediasite/Play/76fd4e37b8744992a05bad4df62db30c1d. Accessed 8 July 2019.
Lund University. 3-D Mammography Detected 34% More Breast Cancers in Screening. Medical Xpress, medicalxpress.com/news/2018-10-d-mammography-breast-cancers-screening.html. Accessed 8 July 2019.
Oliver, Tamlyn. “Overshadowed by Pink: Breast Cancer Is Important, but so Are Other Cancers.” Stat, 2 Oct. 2017, www.statnews.com/2017/10/02/breast-cancer-fundraising-research/. Accessed 8 July 2019.
“Patient Education: Medications for the Prevention of Breast Cancer (Beyond the Basics).” UpToDate, www.uptodate.com/contents/medications-for-the-prevention-of-breast-cancer-beyond-the-basics. Accessed 8 July 2019.
Purohit, V. “Can Alcohol Promote Aromatization of Androgens to Estrogens?” Alcohol, vol. 22, no. 3, Nov. 2000, pp. 123-27, www.ncbi.nlm.nih.gov/pubmed/11163119. Accessed 8 July 2019.
Study Captures the Importance of Screening Mammography for Women with Breast Reconstructions. University of Michigan Health Lab, labblog.uofmhealth.org/health-tech/study-captures-importance-of-screening-mammography-for-women-breast-reconstructions. Accessed 8 July 2019.
US Female Breast Cancer Deaths by Age (2009-2013). Health Line, www.healthline.com/health/breast-cancer/survival-facts-statistics#1. Accessed 15 July 2019.
“Using HRT (Hormone Replacement Therapy).” BreastCancer.org, www.breastcancer.org/risk/factors/hrt. Accessed 8 July 2019.