What does dying mean? Is dying the moment of the actual death or the steep decline that precedes it? More importantly, how should society deal with death? Dr. Atul Gawande’s Being Mortal addresses these questions as he explores the concept of mortality, challenging our current practices when it comes to taking care of the elderly and exhorting us to focus more on what really matters in the end. As history has progressed, medicine has become better at delaying death, but we have not become significantly better at dealing with death. Dr. Gawande calls for a revolutionizing of the current system to better help patients as they reach the end of their lives.

Dr. Atul Gawande
No matter what doctors do, death is eventually inevitable. Whenever we have a fall, medicine can pick us back up, but, after a certain age, we never reach the level of health we previously held. Our health trajectory just points downward. Philip Roth in Everyman writes that “old age is not a battle; old age is a massacre” (Gawande 55). With chronic diseases, treatment merely prolongs the decline, stonewalling death but not the damage caused by the disease. Our body has fail-safes to withstand normal wear and tear like DNA repair mechanisms or our ability to live with one kidney, but eventually, the damage overwhelms our ability to heal. All of a sudden, our health gives away. When a patient dies, a doctor has to file an official cause of death; however, with elderly patients, there is no one true cause. Dr. Gawande contends that fighting battles on various different medical fronts, the real cause is just old age. In the words of geriatrician Dr. Felix Silverstone, “‘we just fall apart’” (35).
Geriatricians are physicians specialized to treat old age. The biggest danger in old age is losing the abilities one currently has, and the job of a geriatrician is to preserve function for as long as possible to afford the patient as much independence as possible. The job of a geriatrician revolves around making old age easier to deal with, which is often overlooked by other physicians. One study split a group of elderly patients to be assigned a geriatrician or their usual physician. What they found was that while the incidence of death was similar, the rates of disability and depression were lower among the geriatrician group. Furthermore, significantly fewer of the geriatrician’s patients were sent to nursing homes. Dr. Gawande notes that if geriatricians were a medical device, we would be clamoring for them to be given to every elderly patient out there. Instead, geriatrics divisions are closing down around the country and the number of geriatricians who are entering the field cannot hope to replace those who are retiring.
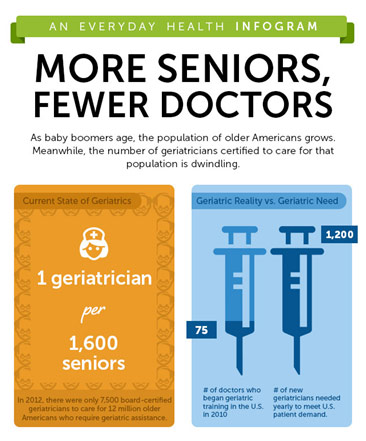
Geriatrician Shortage in the US
Working with a neurosurgery team as an intern, Dr. Gawande met a patient whose metastatic pancreatic cancer had spread to his spine. Despite knowing that the surgery to remove the spinal tumor would not cure him or even reverse his paralysis, that the surgery carried a substantial risk of death especially in his current precarious state, the patient chose surgery. He died from the complications of the surgery. For something that could not be cured, doctors offered treatment. Dr. Gawande comments that doctors are often overly optimistic: 63% of physicians in one study overestimated the time their terminally ill patients had. When dealing with mortality, physicians often fall back to optimism, not wanting to disappoint their patient’s expectations or challenge their own competence by seemingly “giving up.” Competence gives doctors satisfaction and a sense of fulfillment, but death challenges this competence. Thus, doctors do not like to admit the ceiling of their capabilities, so they offer some more last-ditch treatment instead of what the patient really needs: comfort. Dr. Gawande notes that “I knew theoretically that my patients could die, of course, but every actual instance seemed like a violation as if the rules I thought we were playing by were broken” (7). Even physicians feel shocked when medicine does not work like it is supposed to, when the patient’s life is not saved.
It becomes much easier for doctors and patients alike to cling to a hope-filled fantasy about beating the overwhelming odds than to deal with the likely inevitable. There is nothing necessarily wrong with hope. There is something wrong with hope impeding clinical decision making. For instance, Gawande notes the jaw-dropping statistic that “more than 40 percent of oncologists admit to offering treatment that they believe are unlikely to work” (167-68). Furthermore, there is something wrong with not even discussing the more likely scenario and not having that hard conversation about potential end-of-life.
In fact, not having these end-of-life discussions may be quantifiably hurting patients. In one study, half of the patients with Stage IV lung cancer were, in addition to their usual treatment, assigned a palliative care specialist to discuss their goals and priorities among other things. Remarkably, those who met with the palliative care specialist actually survived for 25% longer. When doctors have this end-of-life discussion, it truly helps patients shift their horizons and focus in on the things of importance to them like spending time with family or enjoying the little things in life. While having this end-of-life discussion can be extraordinarily beneficial, it also takes an extraordinary amount of time and effort. It requires giving the patient time to process what the physician is saying. It requires listening to the patient and understanding what is important to them. It is indeed much easier to give that patient some hopeless therapy than to confront their mortality and the limits of medicine’s capabilities. However, doctors must have the wisdom to know when to shift from fighting for time to fighting for the patient’s quality of life. Dr. Gawande writes that death will always win the war, so we need to have a general who understands when to surrender, who “understands that the damage is greatest if all you do is battle to the bitter end” (187).
End-of-Life Discussions: The Elephant in the Room
At the end of our lives, we hope to maintain some autonomy and freedom, but oftentimes, the institutions where we send our elderly fail to prioritize these values. Dr. Gawande’s grandmother-in-law Alice was living independently in her own home even at 84, but she moved to an independent living apartment facility after some episodes of severe disorientation. The design of the facility was to make living safer with nurses giving medication and dieticians controlling the food, but these artifacts just made Alice feel in less and less control of her life. After falling and breaking her hip, she was confined to a wheelchair and was moved to the nursing unit, which was even more confining. Alice did everything only when the nurses told her to do so. When should she bathe? When should she eat? Those were dictated by the schedule. Furthermore, by keeping her in hospital clothes most of the time, she was stripped of her identity. Dr. Gawande compares these kinds of facilities to prisons. They are separated from the community at large with a central authority controlling all aspects of the inmate’s life. Inmates are all treated the same, effectively dehumanizing them. The thing is that these institutions are set up to meet societal needs such as putting our elderly in a safe place, unloading the burden of taking care, or worrying about the elderly off the shoulders of the family. Nevertheless, these institutions do not meet the patient’s goals or what is important to the patient; they do not help keep life worth living or sell themselves as a place that values their patient’s choices. These institutions just become a place where the elderly come to die.
When Dr. Silverstone, the geriatrician mentioned earlier, moved into a retirement community, a sense of purpose pushed him through. He made a journal club for other retired physicians and mentored a young geriatrician. He was also taking care of his wife Bella who was dealing with eyesight and hearing loss as well as memory problems. As Bella’s health steadily declined, Felix could no longer take care of her on his own, so she was moved to the nursing floor of the community. The problem, however, was that she was being treated as a patient, not a person. There was a certain way she liked her food cut, a certain way she liked to be dressed for instance. When she tried explaining it to the nursing staff, they either did not get it or did not care. To them, she was just another patient who they needed to quickly though.

A Minnesota Nursing Home
Old age often makes independence difficult, but we do not have to make it an impossibility. While nursing homes are made to exert complete control over their patients, a quality alternative exists with assisted living, which offers both privacy and autonomy. With assisted living, the elderly are not reduced to patients but are tenants who have control over, for example, who comes into their apartment and when they do so. The basic services of assisted living are quite similar to that of a nursing home, but the power dynamic is fundamentally dissimilar. The tenants can take the risks they want to instead of being restricted and micromanaged by the staff. They have control over their health and their lives. If a patient does not want to take a medication one day so they can feel lucid, then they can do so because that is their choice. Dr. Gawande asserts that we all have a fundamental desire for autonomy, for the ability to continue to be able to write our own stories instead of having them written for us. When compared to nursing homes, the elderly in assisted living were shown to have increased physical function and decreased rates of depression. Unsurprisingly, a little freedom goes a long way.
Dr. Bill Thomas conducted an experiment in a nursing home in upstate New York in 1991. To combat the three plagues of “boredom, loneliness, and helplessness,” he wanted to bring in some life to the nursing home (116). He replaced the artificial plants with real ones, eventually setting up a thriving garden. More remarkably, however, after lobbying the nursing home and state officials, he brought in two dogs, four cats, and one hundred parakeets. Indeed, the animals Dr. Thomas brought into the nursing home renewed the spark of life in the patients. Residents who barely uttered a word began taking an active interest in the project, naming the birds, taking the dogs for a walk, feeding the cats, etc. The number of prescriptions given to the patients fell to one half of what they once were; deaths fell by fifteen percent. Dr. Thomas hypothesized that caring for these animals, for example, gave these patients a reason to live. It was something that went beyond them and their singular life. It gave these patients a purpose.
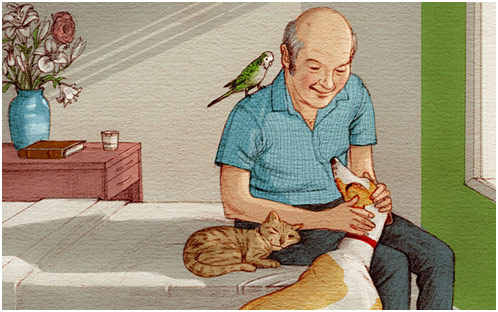
Dr. Bill Thomas’ Nursing Home
In the hospital, patients make sacrifices to be able to extend their life for as long as possible. They endure suffering and pain through surgery, for instance, to hopefully live longer. Gawande contends that having courage in medicine with regards to mortality has two meanings: doctors must have the courage to have the hard conversations about the patient’s end-of-life, and then, they must have the courage to act on this, to start fighting for the patient’s quality of life instead. Many often enter medicine, hoping to save lives but maximizing the quality of life is as important, if not more. Medicine is not just to “ensure health and survival”; it is to “enable wellbeing,” or, in other words, “the reason one wishes to be alive.” (259)
REFERENCES
Being Mortal. Amazon, www.amazon.com/Being-Mortal-Illness-Medicine-Matters/dp/1250081246. Accessed 30 July 2019.
Can live in a Nursing Home Be Made Uplifting and Purposeful? The Telegraph, www.telegraph.co.uk/culture/books/11139446/Can-life-in-a-nursing-home-be-made-uplifting-and-purposeful.html. Accessed 30 July 2019.
The elephant in the room. 27 Oct. 2014. The New Yorker, www.newyorker.com/cartoon/a11766. Accessed 30 July 2019.
Gawande, Atul. Being Mortal: Medicine and What Matters in the End. New York, Macmillan Audio, 2014.
Llewellyn, Tim. Atul Gawande. Monmouth University, www.monmouth.edu/events/event/being-mortal-medicine-and-what-matters-in-the-end/. Accessed 30 July 2019.
More Seniors, Fewer Doctors. Be Seen Get Screened, www.beseengetscreened.com/blog/more-seniors-fewer-doctors-the-geriatrician-shortage-in-the-us. Accessed 30 July 2019.
Robertson, Tom. Residents at the Havenwood Care Center in Bemidji. MPR News, www.mprnews.org/story/2008/05/20/nursinghomedecline. Accessed 30 July 2019.