A few years back, I took a Stanford CME Course on dealing with several life-threatening emergencies. First aid plays a crucial role in our healthcare system, helping bridge the gap between the onset of an acute, potentially fatal event and the arrival of emergency medical services. First aid can and does save lives, underscoring the importance of learning this vital life skill. In this blog post, I will be discussing cardiac arrest, anaphylaxis, asthma, and seizures to help explain potential first aid for these conditions. It is important to note that none of this is intended as medical advice, and the information described here should be learned through formal training before implementation. This post is written for educational purposes alone.

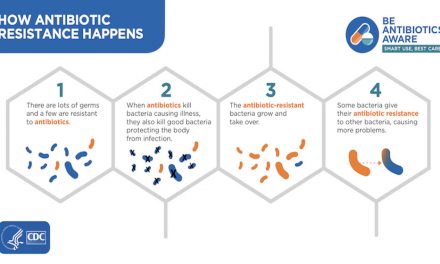
Imagine a middle-aged man with chest pain loses consciousness. The most likely diagnosis here is probably cardiac arrest given that over 350k Americans experience cardiac arrest every year. As always, the first step should be getting help, which may involve getting additional personnel, a crash cart with an automatic external defibrillator (AED), and calling 911. You should then check for a pulse, using the carotid artery in the neck or the radial artery in the arm. In case you do not know how to check for a pulse, you can check if the person is still breathing by looking for chest rise and fall. If the pulse or breathing cannot be ascertained within 10 seconds, you should assume the person does not have a pulse or is not breathing and position their back onto a hard surface to begin CPR. With hands interlocked, one on top of the other, you should compress the lower half of the sternum (breastbone) by about two inches, pushing hard and fast at a compression rate of 100 compressions per minute. The famous song “Stayin’ Alive” can help maintain that rate. If done correctly, these compressions can give a person a systolic blood pressure of 60-80 mm Hg, providing life-sustaining circulation to vital organs.
After every 30 compressions, you should give the person two ventilation, breathing into their mouth. Tilt their head back so that their chin points up and give a one-second-long breath, enough to see visible chest rise in the patient. You should avoid rapid, forceful breaths, which can cause aspiration (vomit, food, or liquid entering the airway) or regurgitation. 5 cycles of CPR should be administered every 2 minutes with one cycle consisting of 30 compressions and 2 breaths. On top of that, it is important to avoid poor quality or interrupted CPR, so people should switch out as they become tired. If/when an AED arrives, it should be used to help get the patient out of cardiac arrest. An AED works by delivering an electric shock that eliminates all cardiac electrical activity. If there is still viable cardiac tissue, the heart’s natural pacemaker will resume electrical activity, restoring normal rhythm. One pad of the AED should be placed on the upper right chest with the other pad should be placed on the lower left chest. The AED will determine if a patient is in a shockable rhythm and if a shock is necessary. If both answers are yes, then the AED will administer a shock; nobody should be touching the patient at that time.
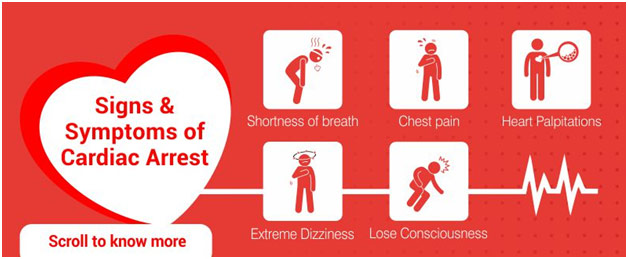
Symptoms of Cardiac Arrest
Anaphylaxis is a severe life-threatening allergic reaction that mandates immediate care. You can make the diagnosis if the person has trouble breathing (respiratory compromise) or reduced blood pressure (cardiovascular compromise) with acute illness of the skin or tissue (eg. rashes, hives). Anaphylaxis involves an allergen trigger, and that allergen should be removed if still in contact because, the longer the patient is exposed, the more severe their condition will be. Next, you want to position the patient with legs elevated relative to the heart to help maintain blood pressure because anaphylaxis can lead to the loss of 25% of blood volume from the intravascular space. In fact, the patient can go into cardiac arrest if this step is not taken. If possible, an EpiPen should be procured. Epinephrine, or adrenaline, helps decrease fluid leak, decrease swelling, raise cardiac output, and decrease how blocked the airway is. The EpiPen should be injected directly into the person’s lateral thigh without any delay as there are no contradictions to epinephrine and the needle can go through fabric. If the person immediately gets better, they should still go to the emergency room because epinephrine is merely a temporary solution. If the patient is not getting better, the dose should be repeated in 5-15 minutes. In patients with anaphylaxis, care needs to happen rapidly because death can occur in as little as five minutes and typically in less than an hour. Time to treatment is an important predictor of mortality in the form of pulmonary collapse in the case of food allergens and cardiovascular collapse in case of stings, bites, venom, or medication allergens.
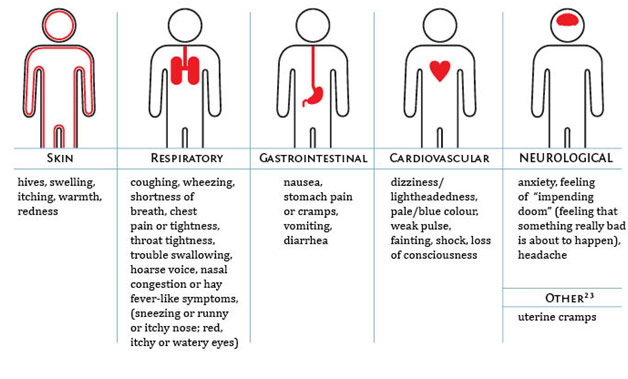
Symptoms of Anaphylaxis
Another emergency is a severe asthma attack because that can cause a patient to be unable to breathe. Signs of severe asthma include a limited ability to speak because of shortness of breath and getting in the tripod position with the person leaning forward, hands on their knees. The patients may become confused or lethargic and start to wheeze or cough a great deal. If the asthma attack is particularly severe, the patient might have a silent chest where you do not even hear wheezing because they are not moving any air. The first step should be to position the patient so that they are sitting up and then to gather all emergency equipment available, which might include albuterol (inhaler) and a bag-mask. Albuterol is a beta-agonist that can provide rapid bronchodilation or the opening of the airway. For a metered-dose inhaler with a spacer, the patient should get 4-8 puffs of albuterol every 20 minutes. You should also help the patient breathe with a bag-mask, pumping the bag at a rate just enough to make the chest rise with enough time between ventilation to allow the chest to fall again. Ventilating too fast may cause injury.
Imagine a patient with chronic headaches stares off into space, falls slowly, and starts exhibiting jerking movements. The most likely diagnosis for this patient is a seizure, and the first thing you should do is put the patient in the left lateral decubitus position where the patient are lying down on their left side. This position reduces the risk of life-threatening aspiration. Additionally, you should clear any furniture or anything the patient might hit while seizing in order to protect them. You should also never put anything into the mouth of a seizing patient because it can cause the seizing person to choke, or the patient might bite it in the case of a finger. Afterward, the most important thing you can do is to watch and wait because the seizure will most likely stop on its own. However, if the seizure continues for over five minutes or the person has a second seizure before recovering from the first one, the patient might develop apnea (low respiratory rate) or become cyanotic (bluish discoloration of lips and nails), meaning the person is not getting enough oxygen. In this case, you should open the airway using a head-tilt, chin-lift maneuver before using a bag-mask at a rate of 10-12 breaths per minute, again being careful not to hyperventilate the patient.
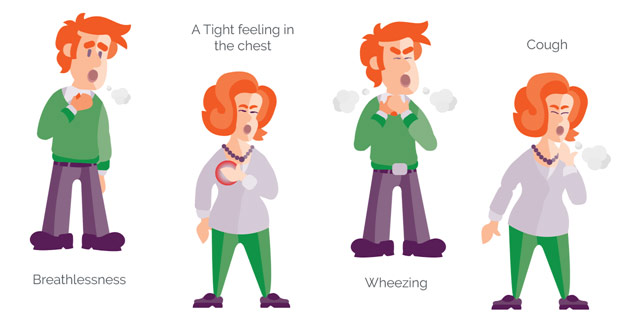
Severe Asthma Symptoms
In my belief, everyone should take a first aid course because the investment is minimal relative to the potential benefit of saving a life. Here, we discussed a couple of life-threatening emergencies and the very basics of first aid for them as an introduction. I hope this post inspires you to take formal training in first aid if you have not already done so.