In a study by BMJ Quality & Safety, it was estimated that over twelve million Americans were misdiagnosed by their doctors each year. Obviously, this is a statistically significant amount that may not necessarily rooted in the incompetence of the doctors but, rather, in the cognitive biases that doctors fall for when they diagnose a patient. The Patient Safety Network of the US Department of Health and Human Services estimates that “about 75% of diagnostic errors have a cognitive component.” When things get hectic, for example in the emergency department, these errors tend to present themselves more often as doctors rush from one patient to another unable to take a step back to evaluate their work. Today, we will focus on the principle of Occam’s Razor and how it relates to medicine.
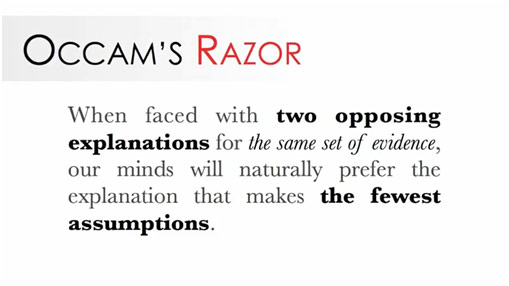
Basis of Occam’s Razor
Medieval philosopher William of Occam serves as the namesake of Occam’s Razor, which is simply another way of saying the common aphorism “when you hear hoofbeats think horses, not zebras.” In other words, the simpler, less-assumption-heavy explanation is often correct. We must just “shave off” less likely or more complicated interpretations for a phenomenon. Another name for Occam’s Razor is Sutton’s Law, named after bank robber Willie Sutton who told the court he robbed banks “because that’s where the money is.” Sutton’s Law simply emphasizes the importance of looking at the obvious reason for something. A nonmedical example of the use of Occam’s Razor is if you see a puddle of water on the ground next to a fallen cup, you might reasonably believe that something knocked a cup of water down. Also possible is that there was minor flooding in just that area and a strong gust of wind blew the cup down. However, this is clearly much less likely. If a student fails a biology test, it is possible that his malicious teacher instructed him wrong in order to protect his job security, but it is simpler and more likely that the student did not study enough. If a friend does not reach the party at the exact moment it is supposed to start, it is possible that she was abducted by aliens on her way there, but it is simpler and more likely that she is just running late. Occam’s Razor is a useful tool because it often does reveal the correct explanation.
Simplicity of Occam’s Razor
Occam’s Razor obviously has clear medical implications as doctors tend to use it to help with diagnostics. If a patient comes in with pain in their head, as a doctor, one should first think the patient has a headache, not a brain tumor. If a 70-year old patient has chest pain, one should think of myocardial infarction rather than pericarditis, inflammation of the sac around the heart. An article in the Journal of the Royal Society of Medicine gives this example in regards to Occam’s Razor.
Imagine a patient presents to casualty complaining of a headache, neck stiffness, fever, and confusion – it is of course perfectly possible that he simultaneously developed a subarachnoid hemorrhage, torticollis, and hepatic encephalopathy. However, Ockham’s razor offers us a single diagnosis that fully accounts for this single presentation and guides us to a diagnosis of meningitis.
Subarachnoid hemorrhage, or bleeding in the space around the brain, would explain the headache. Torticollis, or an abnormal neck position, would explain the neck stiffness. Hepatic encephalopathy, or hepatic failure leading to toxin buildup affecting mental status, would explain the fever and confusion. However, meningitis, an inflammation of the meninges, which protects the brain, would explain all of these symptoms and be more likely than these three disparate diseases developing in the patient at once. Occam’s Razor is all well and good when it works; the problem arises when the doctor thinks of “horses” when the disease is really “zebras.”
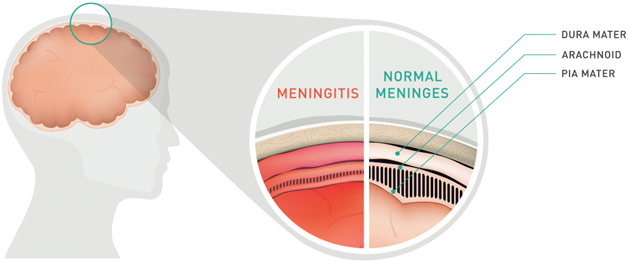
Meningitis Diagram
Hickam’s dictum is attributed to Dr. John Hickam, who said “a man can have as many diseases as he damn well pleases.” To put it simply, the “simpler” explanation of one disease encompassing all the patient’s symptoms may not always be correct because there may be many coexisting conditions present. Take an example of a colon cancer patient coming into the hospital complaining of a fever and cough. On the chest x-ray, the patient has new lung nodules. Instead of jumping to the conclusion that cancer has metastasized to the lung like Occam’s Razor would mandate, if the doctor was following Hickam’s dictum, they would also consider infection, which would look the same as cancer, or a synchronous lung tumor. Although these separate diagnoses may be less likely, it can prove foolish to simply discount them. If the doctor just declares that it is metastasis, the doctor will stop looking for other potential causes of the patient’s symptoms, falling suspect to the potentially deadly satisfaction of search. British surgeon Dr. Charles Saint similarly showed the dullness of Occam’s Razor with his Saint’s Triad, which is the occurrence of the completely separate issues of diverticulosis, gallstones, and hiatal hernia. A 1955 study found that in 14% of patients with hiatal hernia, they also had diverticulosis and gallstones. Some doctors would just follow Occam’s Razor and assume the patient’s symptoms were explained by gallbladder diseases, falling suspect to the satisfaction of the search, leaving the gallstones and diverticulosis undiagnosed.
In an era when people are living longer and longer and developing many chronic illnesses, coexisting conditions will be common, so Occam’s Razor must be used with care so that clinicians do not fall suspect to the satisfaction of search. Occam’s Razor is certainly a good tool to most sustainably use resources, time, and energy towards the most likely diagnosis, yet it should not preclude physicians from keeping their mind open and developing a robust list of differential diagnoses. Occam’s Razor must be balanced with Hickam’s dictum; simplicity should not preclude the reality. If physicians can work the fine line between these two tools, then patients can be better and more realistically diagnosed and treated.
REFERENCES
“Episode 152: Ockham’s Razor Vs. Hickam’s Dictum.” Pharmacy Joe, 2 Jan. 2017, www.pharmacyjoe.com/ockhams-razor-vs-hickams-dictum/. Accessed 19 Mar. 2019.
Furst, John. “Meningitis Diagram.” First Aid for Free, 1 May 2017, www.firstaidforfree.com/what-is-meningitis/meningitis-diagram/. Accessed 19 Mar. 2019.
Heylighen, F. “Occam’s Razor.” Principia Cybernetica Web, 7 July 1997, pespmc1.vub.ac.be/OCCAMRAZ.html. Accessed 19 Mar. 2019.
Kagan, Julia. “Willie Sutton Rule.” Investopedia, 30 May 2018, www.investopedia.com/terms/w/willie-sutton-rule.asp. Accessed 19 Mar. 2019.
King, Jack Preston. “When Occam’s Razor Doesn’t Cut It.” Medium, 7 Nov. 2017, medium.com/@beyondtherobot/when-occams-razor-doesn-t-cut-it-11c185e70a50. Accessed 19 Mar. 2019.
Occam’s Razor. occamsrazorcsueb.wordpress.com/. Accessed 19 Mar. 2019.
Occam’s Razor. 18 Feb. 2010. The Slovak Yankee, mhollick.typepad.com/slovakyankee/2010/02/occams-razor.html. Accessed 19 Mar. 2019.
Palmer, Eddy. “Saint’s Triad (Hiatus Hernia, Gall Stones and Diverticulosis Coli): The Problem of Properly Directing Surgical Therapy.” The American Journal of Digestive Diseases, Dec. 1955, link.springer.com/article/10.1007/BF02886494. Accessed 19 Mar. 2019.
Pilcher, Charles. “Diagnostic Errors and Their Role in Patient Safety.” Kevin MD, 31 Mar. 2011, www.kevinmd.com/blog/2011/03/diagnostic-errors-role-patient-safety.html. Accessed 18 July 2017.
Wardrop, Douglas. “Ockham’s Razor: Sharpen or Re-Sheathe?” Journal of the Royal Society of Medicine, vol. 101, no. 2, Feb. 2008, pp. 50-51, www.ncbi.nlm.nih.gov/pmc/articles/PMC2254462/. Accessed 19 Mar. 2019.
What It’s Really like to Work in a Hospital. 14 June 2017. Foundation Education, www.foundationeducation.edu.au/articles/2017/06/ever-wondered-what-it%E2%80%99s-work-hospital-find-out-here. Accessed 19 Mar. 2019.