A few months back, I took a series of Harvard CME courses on opioid use disorder, a devastating chronic illness that has plagued our nation. In 2014, opioids caused 28,647 deaths, and, that same year, the overuse and misuse of opioids was declared a national epidemic. We can trace some of the origins of the current epidemic to the 1990s where pain was considered a fifth vital sign and thus liberally treated with opioids, which were misleadingly and aggressively marketed as “safe.” Patients who became addicted to prescription opioids slowly built up a tolerance to the drug, leading them to turn to more potent, and illicit, drugs such as heroin, which is often less expensive and easier to obtain. Year after year, opioid overdoses are the number one cause of accidental, preventable deaths, causing more deaths than car accidents or gun violence, yet they continue to plague our nation. In this first part of a two-post series, I hope to explain what exactly opioid use disorder is and offer some thoughts on combatting this epidemic.
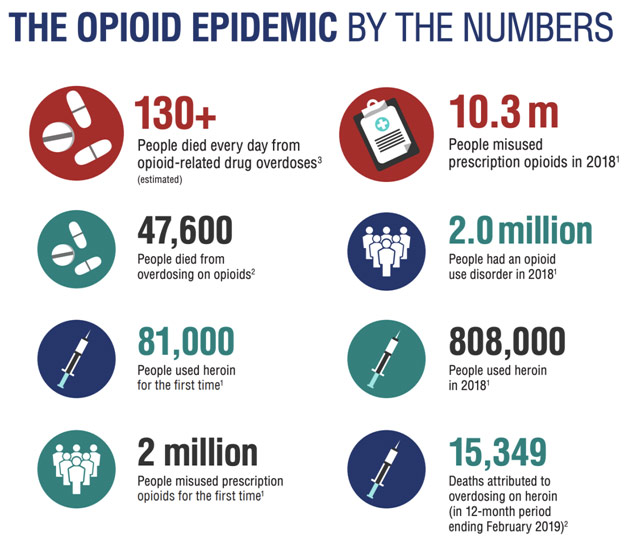
The Statistics of the Opioid Epidemic
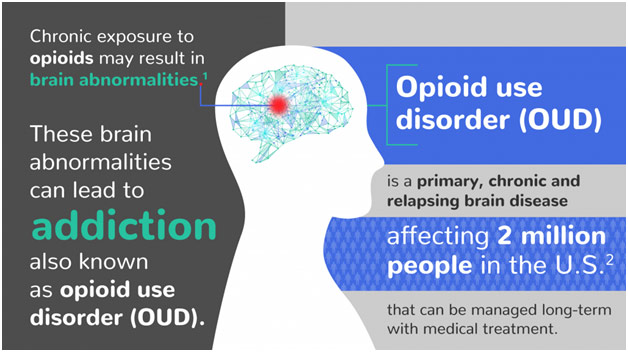
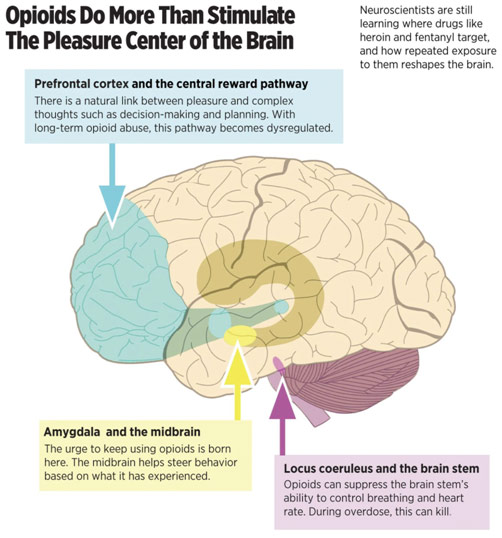
Understanding the neuroscience of addiction is paramount to understanding opioid use disorder. Opioid use disorder, and more generally substance use disorder, is a chronic brain disorder that causes neurological damage. Specifically, it damages our bottom-up salience detection circuit and our top-down cognition and control circuit.
The salience detection circuit helps us understand what is important in our lives. Normally, the neurotransmitter dopamine is released from the ventral tegmental area of the midbrain to the nucleus accumbens to reward us for doing behaviors important to our (or our ancestors’) survival, such as having sex or eating a large meal. Opioids enhance dopamine signals so that our behavior is shaped towards, above all, obtaining and using opioids. Specifically, opioids alter the medium spiny neurons that process stimuli to determine if these stimuli are important to our survival. The hijacking of the salience detection circuit can explain why those with opioid use disorder may stop taking care of themselves, miss days of work, and run through their savings to purchase more opioids: their decision-making process is clouded by opioid-induced structural changes to their brain.
The cognition and control circuit is similarly involved in our making good decisions. The prefrontal cortex of our brains’ frontal lobe is responsible for executive functions such as attention, problem-solving, etc. Opioids deactivate the neurons involved in decision-making and inhibition, which when combined with impairment of the salience detection circuit, creates a devastating cycle of opioid addiction. Patients with opioid use disorder may become intoxicated without self-awareness and overdose because of a lack of control over themselves, which helps explain why it is so difficult for patients to escape their opioid addiction.
Neuroscience of Addiction
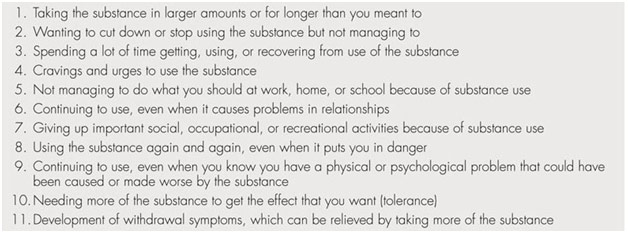
Before discussing treatment for opioid use disorders, we must endeavor to understand first how this chronic disease is diagnosed. The Diagnosis and Statistical Manual of Mental Disorders, or DSM-5, defines substance abuse as a “maladaptive pattern of substance use leading to clinically significant impairment or distress” before listing a series of eleven symptoms. The manifestation of two or more of those symptoms in a 12-month period provides evidence of a substance use disorder. These eleven symptoms fall under four major categories: impaired control over drug use (eg. inability to control the use of the substance despite the desire to do so), social impairment due to drug use (eg. inability to fulfill major obligations), risky drug use (eg. recurrent use in situations in which it is physically hazardous), and pharmacological effects on biological functioning (eg. building tolerance so that markedly diminished effects with the same amount of substance). 2-3 positive responses to the eleven criteria are indicative of a mild substance use disorder, 4-5 positive responses are indicative of a moderate substance use disorder, and 6 or more positive responses are indicative of a severe substance use disorder. The patient is said to be in early remission if none of the criteria, aside from craving the drugs, have been met for a minimum of three months; the patient is in sustained remission if none of the criteria, aside from cravings, have been met for a minimum of twelve months.
Eleven DSM-5 Criteria for Substance Use Disorder
Treatment for opioid use disorder comes in all sorts of varieties because of the complex manifestation of this chronic disease. In this post, I want to focus on opioid maintenance therapy and psychosocial treatments for opioid use disorder.
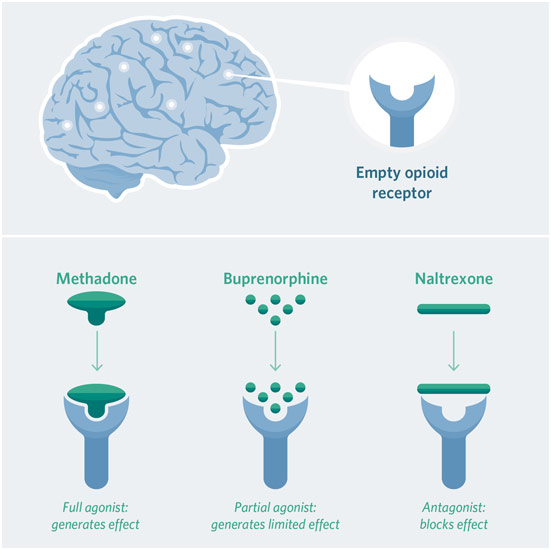
Opioid maintenance therapy is generally conducted with either methadone or buprenorphine and is designed to help patients with high drug tolerance. Methadone and buprenorphine serve as crutches for their brains to recover, minimizing withdrawal symptoms and cravings for opioids. Methadone, a full mu-opioid agonist, works by occupying the same receptors that the opioids bind to, blocking euphoria from coming from outside opioids. Early research has shown that there are minimal side effects associated with methadone and that there is no change intolerance over time. Indeed, since the same receptors are still activated, the patient does not have opioid withdrawal or cravings. For that reason, however, methadone has the potential for being abused and is thus highly regulated, being almost always only administered in a clinic setting. However, if patients meet a federal eight-point criterion, which includes being abstinent from all drugs and alcohol misuse among other things, they may be eligible to take their medications at home. For highly motivated patients, they may even be able to undergo medically-supervised withdrawal from methadone.
Buprenorphine, on the other hand, is a partial mu-opioid agonist, so, while it binds to the same receptors as methadone, it actives them only partially. As a result, it has a greater safety profile than methadone while still reducing cravings and withdrawal symptoms for opioids. Buprenorphine is often combined with naloxone, commercially known as the overdose reversal drug Narcan because the antagonist naloxone blocks opioids from activating the receptors at all. When suboxone, the combination medication, is given sublingually (under the tongue), naloxone does not have any significant effect. The naloxone would only kick in if someone tried to inject the suboxone intravenously by causing unpleasant withdrawal cravings, which helps to prevent abuse of suboxone. Thus, suboxone both prevents negative reinforcement (craving gone) and positive reinforcement of taking other opioids (heroin does not give any euphoria).
Rarely is a patient only on maintenance therapy, however. Those with opioid use disorder are nearly always encouraged to also undergo psychosocial treatment through individual and group therapy. Indeed, given the high relapse rates of short term detoxification programs and the underutilization of maintenance therapy, psychosocial treatment plays an important role in treating substance use disorder in its own right. There are various modalities of interventions. Drug counseling seeks to teach patients to relapse prevention skills as well as how to manage cravings. Cognitive Behavioral Therapy tries to break the link between drug cues and drug cravings/use, helping patients avoid triggers and cope through problem-solving to increase abstinence. Contingency management uses positive reinforcement, rewarding the patient for behaviors related to opioid abstinence, and other adherence targets. Peer support groups, such as sober social networks, relapse prevention groups, and 12-step meetings, can be quite beneficial by providing the patient with a community.
Receptor Activity for Methadone, Buprenorphine, Naltrexone
In the US, it costs over $75 billion a year to pay for opioid use disorder in terms of ER costs, opioid-related deaths, lost productivity, criminal justice system involvement, etc. That number does not even include the societal costs on the families of those with opioid use disorder. Making a dent in the opioid epidemic necessitates expanding treatment options for those addicted to opioids. As of now, only 50% of addiction treatment centers offer medication: that number must be higher. Furthermore, we need to reduce the stigma behind opioid use disorder so that patients may openly discuss their condition with their doctor without fear of judgment. Opioid use disorder should be treated like diabetes, hypertension, or any other chronic illness: patients must always be given the same dignity and compassion. While the current state of affairs is far from ideal, we are living in hopeful times. Prevention and education of medical professionals about risk factors for addiction and how to treat pain, treatment expansion specifically targeting opioid agonist medications, and three, overdose reversal with intranasal naloxone known as Narcan.
REFERENCES
DSM-5 Criteria for Substance Use Disorder. The Mind’s Machine, 2e.mindsmachine.com/figures/04/Table.04.04.html. Accessed 23 Nov. 2019.
Haydon, Iam. Opioids Do More than Stimulate the Pleasure Center of the Brain. The Philadelphia Inquirer, www.inquirer.com/philly/health/addiction/what-science-knows-about-how-opioids-reshape-your-brain-20180724.html. Accessed 23 Nov. 2019.
How OUD Medications Work in the Brain. The Chris Atwood Foundation, www.chrisatwoodfoundation.org/single-post/2018/07/25/Medications-to-treat-opioid-addiction. Accessed 23 Nov. 2019.
“Identification, Counseling, and Treatment of OUD – 8 CME Credits.” Harvard Medical School, cmeonline.hms.harvard.edu/courses/course-v1:HMSCMEOnline+OUDEP2+2T2019/about?utm_source=cme-catalog. Accessed 23 Nov. 2019.
“Managing Chronic Pain in Adults with or in Recovery from Substance Use Disorders.” NCBI, ncbi.nlm.nih.gov/books/NBK92053/table/ch2.t5/. Accessed 23 Nov. 2019.
“Medications to Treat Opioid Use Disorder.” National Institutes of Health, www.drugabuse.gov/publications/medications-to-treat-opioid-addiction/what-are-misconceptions-about-maintenance-treatment. Accessed 23 Nov. 2019.
The Neurobiology of Opioid Dependence. 2018. Braeburn, braeburnrx.com/opioid-use-disorder/. Accessed 23 Nov. 2019.
The Opioid Epidemic by the Numbers. Health and Human Services, www.hhs.gov/opioids/sites/default/files/2019-11/Opioids%20Infographic_letterSizePDF_10-02-19.pdf. Accessed 23 Nov. 2019.
“Opioid Overdose Crisis.” National Institutes of Health, www.drugabuse.gov/drugs-abuse/opioids/opioid-overdose-crisis. Accessed 23 Nov. 2019.
Rudd, Rose, et al. “Increases in Drug and Opioid Overdose Deaths – United States, 2000-2014.” Centers for Disease Control and Prevention, www.cdc.gov/mmwr/preview/mmwrhtml/mm6450a3.htm. Accessed 23 Nov. 2019.
“Understanding Addiction – 8 CME Credits.” Harvard Medical School, cmeonline.hms.harvard.edu/courses/course-v1:HMSCMEOnline+OUDEP1+2T2019/about?utm_source=cme-catalog. Accessed 23 Nov. 2019.