Do you know someone with diabetes, heart disease, or asthma? What would you say if I told you that 78% of people would not want to be a coworker with that person, that 90% would be unwilling to have that person marry into their family? What would you say if I told you that 54% of people think that landlords should be able to deny these people housing, that 64% think that employers should be able to deny them a job? These statistics are actually for patients with substance use disorder, a chronic illness much like diabetes, heart disease, and asthma. As shown by these statistics, there is a significant bias against these patients, and this bias has untold detrimental health consequences. A few months back, I took a series of Harvard CME courses on opioid use disorder, and, in the second part of this two-post series, I hope to unpack the bias against those with drug addiction and the importance of talking about substance use disorder as the chronic illness that it is.
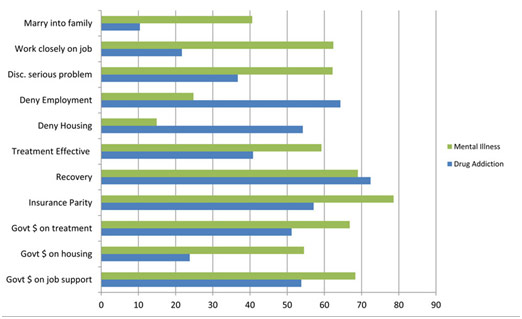
Bias Against Drug Addiction is Greater than Bias Against Mental Illness
Unfortunately, society is not just biased against those with substance use disorder but also against the success of current treatments. For instance, as reported by Barry et al. in a paper in the Psychiatric Service journal, 59% of survey respondents view treatment for substance use disorder as unsuccessful in controlling symptoms, and 28% rejected that people with drug addiction “could, with treatment, get well and return to productive lives.” These numbers are so impactful because they help explain why treatment for opioid use disorder is largely underutilized. While there are over 14,000 treatment facilities for substance use disorder, only 10% of people with this condition get help. This is in spite of the fact that treatment for substance use disorder is highly effective with 50-60% of people receiving treatment achieving sustained remission.
Part of the issue is a bias against the treatment itself. Methadone and buprenorphine maintenance therapy, as explained in Part 1, are the standards of care, yet society still views them unfavorably, seeing it as merely substituting one drug with another, one addiction with another. Stories like a dad being rejected visitation rights to his child since he is undergoing methadone maintenance therapy—not using any illicit drugs—-are all too common. On top of that, when patients relapse, which is part of the nature of chronic conditions, society tends to blame them for that as well. Much like for diabetes, heart disease, or asthma, we need to remember that, while there is no cure, medical management does help and that there will be cycles of active illness and remission. We have to remember that patients do not “fail” treatment; insufficient treatment “fails” patients.
Despite their medical training, physicians are also not immune to bias against patients with opioid use disorder. Physicians tend to avoid patients with substance use disorder, seeing it as too challenging to deal with them, immediately labeling these patients as deceptive and insincere. If forced to meet with them, physicians have significantly shorter meetings with and less empathy for these patients. A physician claiming that a patient with substance use disorder has no desire to change is all too frequent these days. The explicit and implicit bias against patients with opioid use disorder prevents physicians from fulfilling their duty to deliver equal care to all and isolates these patients: this kind of discrimination has been linked to higher rates of dropping out of treatment programs for opioid use disorder for example. Part of the issue here is the lack of specific training with regards to substance use disorder: medical schools have to emphasize treating opioid use disorder as a chronic condition as they train the next generation of physicians. We have to remember that physicians are here to help, not judge.
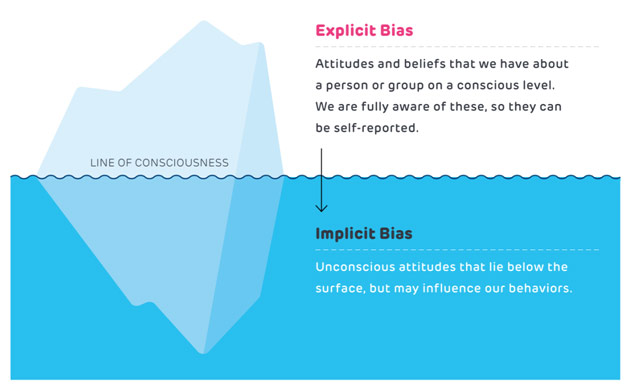
Difference Between Explicit Bias and Implicit Bias
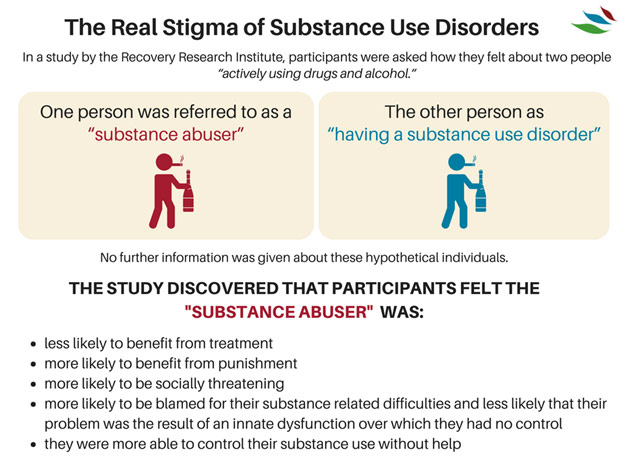
A large portion of the bias surrounding opioid use disorder also comes down to how we speak about it. Our conceptualizations of opioid use disorder tend to associate blame for the condition with the patient, seeing it as a “moral failing.” Calling someone an “opioid abuser” indicates that they are engaging in some sort of willful misconduct, even though opioid use disorder has an important genetic risk factor. Even the word “addiction” carries a highly negative connotation, suggesting a patient’s inability to control themselves. Rather than blaming patients for becoming addicted in the first place, we have to exercise greater compassion and remember that they are addicted to the drugs—they have lost the choice not to take it. Much like how the language around mental health has shifted (and is shifting) from “mentally retarded” to “an intellectual or developmental disability” or from “psycho” to “one with a mental health condition,” the language around addiction must change. Linguist Benjamin Whorf proposed that language determines thought, but, at the very least, language influences thoughts. By being a little more careful with our words, we can tackle the stigma around opioid use disorder in a big way.
Sticks and Stones May Break My Bones, but Words Will Always Hurt Me
The thing is, this stigma around opioid use disorder prevents people from acknowledging and accepting that they may have a problem, preventing patients from seeking out help or from continuing treatment. When we reduce stigma, we encourage more patients with opioid use disorder to seek out treatment and get better. When we treat these patients with the same dignity and compassion as any other patient with a chronic illness, when we listen without judgment, we reduce negative consequences for these patients. Opioid use disorder is a treatable disease of the brain: if we can spread awareness about that simple fact, we can improve the lives of those suffering from this chronic disorder.
References
Barry, Colleen, et al. “Stigma, Discrimination, Treatment Effectiveness, and Policy Support: Comparing Public Views About Drug Addiction with Mental Illness.” Psychiatric Service, vol. 65, no. 10, Oct. 2014, pp. 1269-72, www.ncbi.nlm.nih.gov/pmc/articles/PMC4285770/?holding=F1000&otool=stanford. Accessed 7 Dec. 2019.
Colley, Amy. “Battling Bias: Tales from an Addiction Psychologist.” The Fix, 16 Apr. 2015, www.thefix.com/content/battling-bias-tales-addiction-psychologist. Accessed 7 Dec. 2019.
Lopez, Karla, and Deborah Reid. “https://www.healthaffairs.org/do/10.1377/hblog20170413.059618/full/.” Health Affairs, 13 Apr. 2017, www.healthaffairs.org/do/10.1377/hblog20170413.059618/full/. Accessed 7 Dec. 2019.
“Understanding Addiction – 8 CME Credits.” Harvard Medical School, cmeonline.hms.harvard.edu/courses/course-v1:HMSCMEOnline+OUDEP1+2T2019/about?utm_source=cme-catalog. Accessed 7 Dec. 2019